
CMS has released the 2026 Final Rule for the Quality Payment Program (QPP), continuing its incremental shift toward MIPS Value Pathways (MVPs), adjusting quality and cost strategies, and laying groundwork for future interoperability and digital measures. While 2026 introduces fewer sweeping changes, clinicians and Accountable Care Organizations (ACOs) should take note of important updates across the Merit-Based Incentive Payment System (MIPS) and the Medicare Shared Savings Program (MSSP). Below is a breakdown of the finalized policies and how they may affect you.
MIPS Structure and Participation
CMS is aiming for stability in the MIPS program structure, with few changes to participation options or scoring thresholds in the 2026 performance year.
- Performance Threshold: CMS is maintaining the performance threshold at 75 points through the 2028 performance year (for the 2030 payment adjustment).
- Reporting Options: CMS will continue offering three MIPS reporting options in 2026:
- Traditional MIPS
- MIPS Value Pathways (MVPs)
- APM Performance Pathway (APP)
MIPS Value Pathways (MVPs): Still Optional, But Expanding
While MVP reporting remains optional in 2026, CMS is expanding the framework with new pathways and refinements that signal its growing role in the future of MIPS.
Six new MVPs have been added for 2026:
- Diagnostic Radiology
- Interventional Radiology
- Neuropsychology
- Pathology
- Podiatry
- Vascular Surgery
All existing 21 MVPs have been updated to align with changes to the quality and improvement activity inventories.
MVP Reporting
Beginning with the CY 2026 performance period, multispecialty groups will no longer be able to register as a group to report an MVP. Instead, multispecialty groups that wish to participate in an MVP must register and report at the subgroup, individual, or APM Entity level.
CMS finalized an exception to this policy for multispecialty small practices. Specifically:
- Multispecialty groups with the small practice special status (15 or fewer clinicians) may continue to register to report an MVP as a group.
- Multispecialty groups with the small practice special status aren’t required to register as subgroups if they don’t want to report as individuals.
CMS defines a single specialty group as a group that consists of clinicians in one specialty type or clinicians involved in
a single focus of care. Groups will self-attest their specialty composition (either single-specialty or multispecialty) during MVP registration, rather than CMS making that determination.
Qualified Clinical Data Registries (QCDRs) and Qualified Registries will be given one year after an MVP is finalized before they are required to support it fully, providing more time for technical implementation.
Quality Category: Streamlining Measure Inventory and Policy Refinements
CMS has finalized moderate updates to the Quality performance category in 2026, including adjustments to the measure inventory, measure definitions, and scoring methodologies. These changes reflect a continued emphasis on meaningful quality improvement while reducing redundancy.
The Quality measure inventory changes include:
- 5 new quality measures (including 2 eCQMs)
- 10 existing measures have been removed
- 30 existing measures have been substantively updated
A list of the new measures, along with their collection types, is outlined in the table below.
| New Quality Measures | Collection Type |
| #513 Patient Reported Falls and Plan of Care American Academy of Neurology | MIPS CQM |
| #512 Prevalent Standardized Kidney Transplant Waitlist Ratio (PSWR) | MIPS CQM |
| #514 Diagnostic Delay of Venous Thromboembolism in Primary Care | eCQM |
| #515 Screening for Abnormal Glucose Metabolism in Patients at Risk of Developing Diabetes | eCQM |
| #516 Hepatitis C Virus (HCV): Sustained Virological Response (SVR) | MIPS CQM |
Several measures have been removed from the quality measure inventory for next year.
| Quality Measures to be Removed in 2026 | Collection Type |
| #185 Colonoscopy Interval for Patients with a History of Adenomatous Polyps – Avoidance of Inappropriate Use | MIPS CQM |
| #264 Sentinel Lymph Node Biopsy for Invasive Breast Cancer | MIPS CQM |
| #290 Assessment of Mood Disorders and Psychosis for Patients with Parkinson's Disease | MIPS CQM |
| #322 Cardiac Stress Imaging Not Meeting Appropriate Use Criteria: Preoperative Evaluation in Low-Risk Surgery Patients | MIPS CQM |
| #419 Overuse of Imaging for the Evaluation of Primary Headache | MIPS CQM |
| #424 Perioperative Temperature Management | MIPS CQM |
| #443 Non-Recommended Cervical Cancer Screening in Adolescent Females | MIPS CQM |
| #487 Screening for Social Drivers of Health | MIPS CQM |
| #498 Connection to Community Service Provider | MIPS CQM |
| #508 Adult COVID-19 Vaccination Status | MIPS CQM |
High Priority Measures
In addition to inventory changes, CMS has removed “health equity” from the definition of high priority measures, narrowing the scope to core clinical domains such as outcomes, safety, and care coordination.
Topped Out Measures
To address limited measure choice in certain specialties and MVPs, CMS will continue to apply alternative benchmarks for 19 topped-out measures, allowing clinicians in those areas to still earn meaningful points.
Claims-based Measures
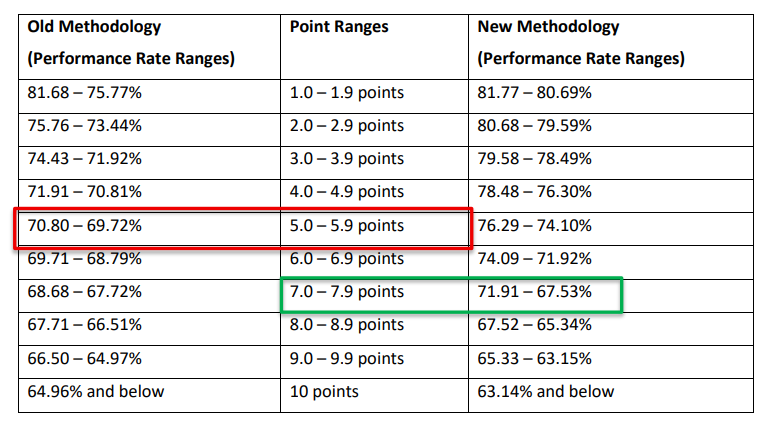
Finally, CMS has revised the scoring methodology for claims-based measures, aligning it with cost measure benchmarking by using median-based scoring and standard deviations to determine performance thresholds. CMS provided the following example to illustrate how the new methodology works in practice: for the Risk-Standardized Acute Cardiovascular-Related Hospital Admission Rates for Patients with Heart Failure measure under MIPS, a performance rate of 70% would have earned 5–5.9 points under the previous methodology, whereas it will now earn 7–7.9 points under the new methodology.
Improvement Activities: Targeted Changes, New Focus on Wellness
CMS has updated the Improvement Activities (IA) performance category for 2026, with a focus on streamlining the inventory and introducing activities that reflect emerging priorities in care delivery.
- 3 new Improvement Activities added, 7 modified, 8 removed.
- The “Achieving Health Equity” subcategory has been retired and replaced with a new subcategory: “Advancing Health and Wellness.”
CMS has adopted the following three new Improvement Activities for the 2026 performance year:
- Improving Detection of Cognitive Impairment in Primary Care
- Integrating Oral Health Care in Primary Care
- Patient Safety in Use of Artificial Intelligence (AI)
CMS has removed eight activities from the inventory for the 2026 performance year.
| Improvement Activities Removed in 2026 |
| IA_ AHE_5 MIPS Eligible Clinician Leadership in Clinical Trials or CBPR |
| IA_AHE_8 Create and Implement an Anti-Racism Plan |
| IA_AHE_9 Implement Food Insecurity and Nutrition Risk Identification and Treatment Protocols |
| IA_AHE_11 Create and Implement a Plan to Improve Care for Lesbian, Gay, Bisexual, Transgender, and Queer Patients |
| IA_AHE_12 Practice Improvements that Engage Community Resources to Address Drivers of Health |
| IA_PM_26 Vaccine Achievement for Practice Staff: COVID-19, Influenza, and Hepatitis B |
| IA_PM_6 Use of Toolsets or Other Resources to Close Health and Health Care Inequities Across Communities |
| IA_ERP_3 COVID-19 Clinical Data Reporting with or without Clinical Trial |
CMS had previously finalized the removal of several improvement activities effective for the 2026 performance period and beyond.
| Improvement Activities Previously Finalized for Removal in 2026 |
| IA_PM_12 Population Empanelment |
| IA_CC_1 Implementation of Use of Specialist Reports Back to Referring Clinician or Group to Close Referral Loop |
| IA_CC_2 Implementation of Improvements that Contribute to More Timely Communication of Test Results |
| IA_BMH_8 Electronic Health Record Enhancements for BH Data Capture |
Promoting Interoperability: Technical Updates to Support Security and Flexibility
While the Promoting Interoperability (PI) category maintains its overall structure and weight in the 2026 final rule, CMS has made several technical updates to strengthen data security, modernize guidance, and add flexibility in response to real-world reporting challenges.
- The Security Risk Analysis measure will now require an additional attestation confirming that clinicians conducted risk management activities, as outlined under the HIPAA Security Rule.
- Clinicians will be required to use the updated 2025 SAFER Guides for their self-assessments under the High Priority Practices measure.
- The Public Health and Clinical Data Exchange objective has been modified by adopting a new optional bonus measure: the Public Health Reporting Using TEFCA measure. The measure is 1 of 4 available bonus measures under the Public Health and Clinical Data Exchange objective, in which a maximum of 5 points can be earned if reporting one, more than one, or all
optional bonus measures.
PI Measure Suppression
In response to operational barriers, CMS is suppressing the Electronic Case Reporting measure for the 2025 performance period due to CDC delays in onboarding new providers and public health agencies.
To proactively address similar issues in the future, CMS also adopted a new measure suppression policy for the PI category. This will allow CMS to suppress PI measures when unexpected challenges make compliance infeasible or unfair for clinicians.
Cost Category: Stable Inventory, More Insight Into Future Measures
The Cost performance category remains largely unchanged in the 2026 final rule, but CMS is made refinements that aim to improve fairness and provide more transparency for future cost scoring.
- No new cost measures have been adopted, and none are being removed. The total number of cost measures remains at 35 for the 2026 performance year.
- CMS has updated the Total Per Capita Cost (TPCC) measure to limit instances where TPCC is attributed to highly specialized groups based solely on billing of advanced care practitioners.
- Looking ahead, CMS finalized a 2-year informational-only feedback period for any new cost measures finalized in future years. During this time, clinicians will see performance feedback without the measure contributing to their MIPS final score—giving practices time to understand and adapt before any financial impact.
APMs & ACOs: More Flexibility, Better Alignment with Attribution
CMS has finalized modest but meaningful updates to APM and ACO participation in the Quality Payment Program, with a focus on improving flexibility in QP determinations and reducing reporting burdens for Shared Savings Program ACOs.
- Advanced APMs
- For Qualifying APM Participant (QP) status, CMS will begin making determinations at both the individual clinician level and the APM Entity level, offering more granular eligibility tracking.
- The QP calculation will be expanded to include all Covered Professional Services, not just E/M services, for better representation of participation.
- APP Plus Measure Set
- Within the APP Plus measure set, CMS has removed the Screening for Social Drivers of Health (Quality ID 487).
- Starting in performance year 2027, Shared Savings Program ACOs will be required to use a web mail phone approach for the CAHPS for MIPS Survey, replacing the current mail phone method to help improve response rates.
- Medicare Clinical Quality Measures (CQMs)
- For ACOs reporting Medicare CQMs, CMS has revised the definition of eligible beneficiaries beginning in performance year 2025 and for subsequent years. Under this policy, a beneficiary would be considered eligible if they received at least one primary care service during the applicable performance year from an ACO professional who is a primary care physician, a specialist included in ACO assignment methodology, or a physician assistant, nurse practitioner, or clinical nurse specialist. This change is intended to increase alignment with the ACO’s assignable population, thereby simplifying patient matching and reducing administrative burden.
- Health Equity Adjustment
- Beginning in performance year 2026, the health equity adjustment applied to ACO quality scores will be discontinued. Additionally, the terminology associated with the adjustment and related concepts has been revised for the 2023 through 2025 performance years.
- Extreme and Uncontrollable Circumstances (EUC)
- CMS has expanded the Shared Savings Program’s quality and financial EUC policies to include ACOs impacted by cyberattacks, such as ransomware or malware, starting in performance year 2025 and beyond.
Final Thoughts
Traditional MIPS remains in place for 2026, but CMS is steadily advancing MVPs as the long-term direction of the program. Clinicians should review the final changes across the MIPS performance categories, as updates or removals may impact scoring. For ACOs, updates to Medicare CQM reporting are intended to ease burden and improve alignment with assigned populations, reflecting CMS’s broader shift toward more streamlined and data-driven performance measurement.
Leave a comment