
2020 MIPS performance feedback reports, which include MIPS final scores and payment adjustment information, are now available. Clinicians and groups should carefully review their reporting results. Any positive or negative payment adjustment will apply to their 2022 Medicare Part B payments for covered professional services. A targeted review can be requested until November 29, 2021, if clinicians believe an error was made in their 2022 MIPS payment adjustment calculation.
What’s in the 2020 Performance Feedback?
The MIPS performance feedback will include a summary of the data clinicians or groups submitted to CMS for the 2020 performance year and their reporting results. Performance feedback will be available for each associated practice at which a clinician was eligible in 2020 and includes the following information:
- 2020 MIPS final score
- 2022 MIPS payment adjustment
- Final performance category scores and weights for Quality, Cost*, Promoting Interoperability, and Improvement Activities
- Measure-level performance data and scores
- Any bonus points for complex patients
*CMS reweighted the Cost category from 15 percent to zero percent for the 2020 performance period for all MIPS eligible clinicians to provide additional COVID-19 relief. The Cost points will be redistributed to other MIPS categories.
How Do Clinicians Access Their 2020 MIPS Performance Feedback Report?
MIPS performance feedback reports are available from CMS, but MDinteractive can assist clinicians with accessing their reports and interpreting the results if they have an MDinteractive account.
- If you previously granted us permission to access your reports, we have already uploaded them to your MDinteractive account. Just click the green “QPP Performance Feedback” icon on your 2021 MIPS dashboard then click “2020 QPP Feedback” to view your 2020 results now.
- If you have not already given us access, please follow the steps below:
Steps to Grant MDinteractive Permission to Obtain Your Reports:
| New Requests | Pending Requests* |
| Log into your MDinteractive account at www.mdinteractive.com | Log into your MDinteractive account at www.mdinteractive.com |
| Click on the blue "QPP Performance Feedback" icon on your dashboard. | Click on the yellow "QPP Performance Feedback" icon on your dashboard. |
| Complete the steps. | Complete the steps. |
*A yellow “QPP Performance Feedback” button on your dashboard means the request is pending and you need to take further action to grant MDinteractive access to your reports.
Important: If your practice has several users with QPP accounts, only the user with the role “Security Official” will receive an email from QPP to give permission to MDinteractive to access your performance feedback report.
Did the COVID-19 Pandemic Impact the Results?
CMS implemented several policies for the 2020 performance period in response to the COVID-19 pandemic.
- CMS applied the MIPS automatic extreme and uncontrollable circumstances (EUC) policy to all MIPS eligible clinicians participating in MIPS as individuals for the 2020 performance period.
- Clinicians who didn’t submit any data, or who only submitted data in one performance category, will automatically receive a neutral payment adjustment in 2022.
- Any performance category for which an individual clinician didn’t submit data is weighted at 0% for the 2020 performance year.
- CMS also reopened the EUC application to individuals, groups, and APM Entities.
- Approved applications will reweight performance categories to 0% unless data was submitted. Note that for the 2020 performance year, approved applications didn’t void previously submitted data.
- CMS reweighted the Cost performance category from 15% to 0% for the 2020 performance period for all MIPS eligible clinicians regardless of participation as an individual, group, or APM Entity. The 15% cost performance category weight will be redistributed to other performance categories.
How is the Final MIPS Score and Payment Adjustment Calculated?
The final MIPS score is the sum of the performance category scores and any additional bonus points. It will be between zero and 100 points depending on the amount of data reported by the clinician or group. The final MIPS score determines if a clinician or group will receive an upward, downward, or neutral payment adjustment in 2022.
Performance Category Weights and Payment Adjustment Based on Individual Data Submission
The table below illustrates the 2020 performance category reweighting policies that CMS will apply to individual clinicians under the MIPS automatic EUC policy. The automatic policy (and the reweighting below) doesn’t apply to clinicians who participate in MIPS as a group or APM Entity.
|
Data Submitted |
Quality Category Weight |
Promoting Interoperability Category Weight |
Improvement Activities Category Weight |
Cost Category Weight |
Payment Adjustment |
|
No data |
0% |
0% |
0% |
0% |
Neutral |
|
Submit Data for One Performance Category |
|||||
|
Quality Only |
100% |
0% |
0% |
0% |
Neutral |
|
Promoting Interoperability Only |
0% |
100% |
0% |
0% |
Neutral |
|
Improvement Activities Only |
0% |
0% |
100% |
0% |
Neutral |
|
Submit Data for Two Performance Categories |
|||||
|
Quality and Promoting Interoperability |
70% |
30% |
0% |
0% |
Positive, Negative, or Neutral |
|
Quality and Improvement Activities |
85% |
0% |
15% |
0% |
Positive, Negative, or Neutral |
|
Improvement Activities and Promoting Interoperability |
0% |
85% |
15% |
0% |
Positive, Negative, or Neutral |
|
Submit Data for Three Performance Categories |
|||||
|
Quality and Improvement Activities and Promoting Interoperability |
55% |
30% |
15% |
0% |
Positive, Negative, or Neutral |
Performance Category Reweighting Scenarios for Group Reporting
The table below identifies the performance category reweighting scenarios applicable to group participation for the 2020 performance year. Note the table reflects the 0% reweighting of the Cost performance category for everyone in the 2020 performance year.
- The Quality, Improvement Activities, and/or Promoting Interoperability performance categories could be reweighted due to an approved EUC application.
- The Promoting Interoperability performance category could also be reweighted due to clinician type, an approved hardship exception or special status.
|
Reweighting Scenario |
Quality Category Weight |
Promoting Interoperability Category Weight |
Improvement Activities Category Weight |
Cost Category Weight |
Payment Adjustment |
| No additional reweighting from an approved EUC application approved Promoting Interoperability hardship exception, clinician type or special status. | |||||
|
No Cost |
55% |
30% |
15% |
0% |
Positive, Negative, or Neutral |
|
Reweight Two Performance Categories |
|||||
|
No Cost and No Promoting Interoperability |
85% |
0% |
15% |
0% |
Positive, Negative, or Neutral |
|
No Cost and No Quality |
0% |
85% |
15% |
0% |
Positive, Negative, or Neutral |
|
No Cost and No Improvement Activities |
70% |
30% |
0% |
0% |
Positive, Negative, or Neutral |
|
Reweight Three Performance Categories |
|||||
|
No Quality, No Cost, No Improvement Activities |
0% |
100% |
0% |
0% |
Neutral |
|
No Quality, No Cost, No Promoting Interoperability
|
0% |
0% |
100% |
0% |
Neutral |
|
No Cost, No Promoting Interoperability, No Improvement Activities |
100% |
0% |
0% |
0% |
Neutral |
|
Reweight Four Performance Categories |
|||||
|
All performance |
0% |
0% |
0% |
0% |
Neutral |
Bonuses
The final score may also include additional awarded bonuses points for complex patients. CMS doubled the complex patient bonus so clinicians can earn up to 10 bonus points for the 2020 performance year (to be added to the 2020 MIPS Final Score). Additionally, if a clinician or group submitted Quality data in 2020, they could also be eligible for an additional Quality Improvement Score.
Facility-Based Clinicians
Facility-based scoring allows certain clinicians and groups to receive scores in the quality performance category for the 2020 MIPS performance period based on their attributed facility’s Fiscal Year (FY) 2020 performance in the Hospital Value-Based Purchasing (VBP) Program. If a clinician qualified for facility-based scoring, they will see a message on the quality page of their performance feedback showing their QPP Equivalent Quality Score Based on the HVBP Percentile.
Payment Adjustments
The MIPS payment adjustments are applied on a claim-by-claim basis to 2022 Medicare payments made for covered professional services. Payment adjustments are determined on a sliding scale based on a clinician or group’s final score. A final MIPS score of fewer than 45 points would result in a negative payment adjustment, while a score over 45 points would result in a positive payment adjustment. Clinicians are also eligible for an “exceptional performance” bonus if their MIPS score was at or above 85 points.
| Final Score | Payment Adjustment |
| 85.00 – 100.00 points (Additional performance threshold = 85.00 points) |
|
| 45.01 – 84.99 points |
|
| 45.00 points (Performance threshold = 45.00 points) | Neutral MIPS payment adjustment (0%) |
| 11.26 – 44.99 | Negative MIPS payment adjustment (between 0% and -9%) |
| 0 – 11.25 points | Negative MIPS payment adjustment of -9% |
The 2022 MIPS payment adjustments vary between -9% and +1.87%. This means a perfect score of 100 MIPS points would result in a positive payment adjustment of +1.87%. Federal law requires CMS to implement MIPS payment adjustments in a budget-neutral manner. Therefore, any positive payment adjustment may be smaller than expected due to high participation rates in the MIPS program, a large number of scores above the 45 point threshold, and policies CMS implemented in response to COVID-19.
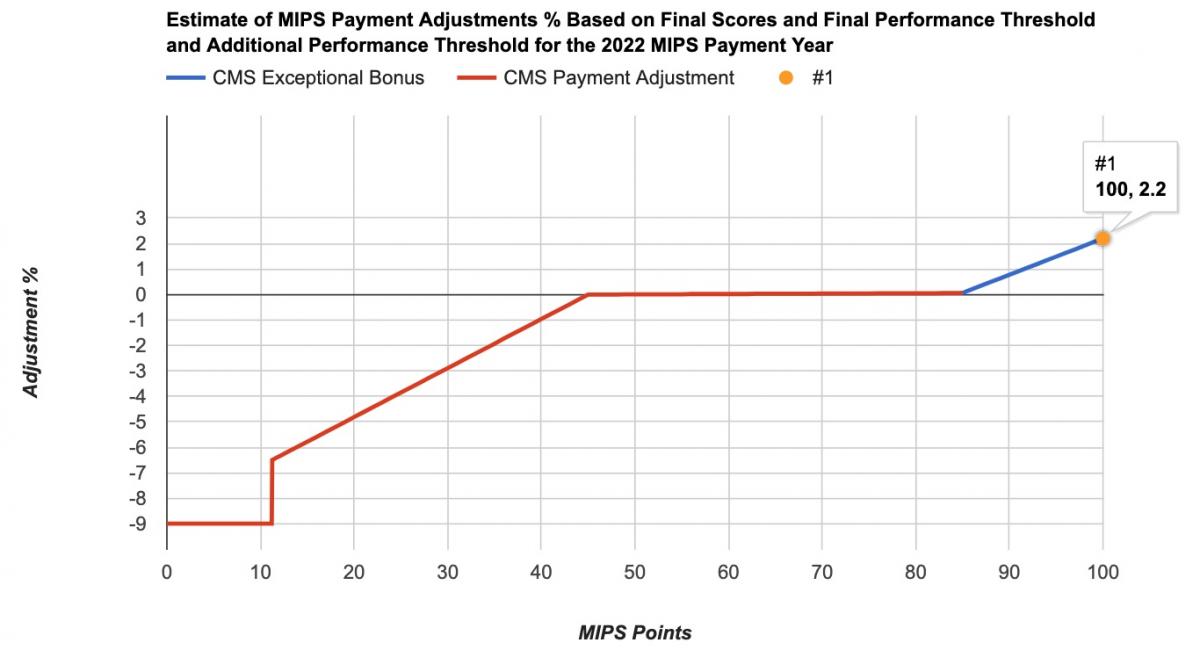
Below are some examples of MIPS scores and matching payment adjustments:
| 2020 MIPS Score | 2022 Payment Adjustment |
| 100 | +1.87% |
| 90 | +0.70% |
| 85 | +0.12% |
| 80 | +0.01% |
| 70 | 0% |
| 60 | 0% |
| 50 | 0% |
| 45 | 0% |
| 40 | -0.87% |
| 30 | -2.89% |
| 20 | -4.81% |
| 10 | -9% |
| 0 | -9% |
MIPS Alternative Payment Models (APMs)
Final MIPS APM performance feedback and payment adjustment information is available to the APM Entity and to the individual clinicians scored under the APM scoring standard. The individual clinician will need to be approved for the clinician role or be approved as a staff user by the APM Entity. Representatives of participant TINs and practices with clinicians scored under the APM scoring standard won’t be able to access the APM Entity’s performance feedback unless they have been approved as a staff user by the APM Entity.
What Should Clinicians Do If They Are Getting a Penalty?
Clinicians should carefully review their performance feedback. Even if a clinician was not MIPS eligible as an individual, but his or her practice reported Medicare Part B claims measures for the Quality performance category in 2020, the clinician could be receiving a penalty because group-level data was not reported for other performance categories to achieve sufficient points to avoid the penalty.
If a clinician doesn't agree with his or her final MIPS score or the payment adjustment information, there is a limited window of time to appeal the decision via a targeted review process. CMS suggests requesting a targeted review as soon as possible if a clinician identifies an error with his or her MIPS final performance feedback and MIPS payment adjustment factor(s). This will help ensure that the correct payment adjustment is applied to the clinician’s claims from the start of the 2022 payment year.
A targeted review can be requested from CMS via a QPP account through 8:00 pm EST on November 29, 2021. It should be requested at the same level as the clinician-reported MIPS (individual or group). Once the targeted review deadline passes, clinicians will no longer have a way to dispute their scores. This is why it is important to access performance feedback reports as soon as they are available.
Examples of reasons for requesting a targeted review:
- Your performance data was submitted under the incorrect Taxpayer Identification Number (TIN) or National Provider Identifier (NPI).
- You qualified for performance category reweighting, due to a special status designation, Promoting Interoperability hardship exception, or extreme and uncontrollable circumstances exception was incorrectly applied.
- Errors or data quality issues for the measures and activities you submitted.
- Eligibility and special status issues.
- Being erroneously excluded from the APM participation list and not being scored under the APM Scoring Standard.
Key Takeaways
Carefully review your 2020 MIPS performance feedback! Your performance feedback can help you determine if improvements are needed for your 2021 MIPS reporting. MDinteractive can assist you with obtaining your performance feedback reports and interpreting the results. If you disagree with your final MIPS score or payment adjustment, you will need to request a targeted review no later than 8:00 pm EST on November 29, 2021.
Leave a comment