On December 1, 2020, CMS released the 2021 Quality Payment Program (QPP) Final Rule under the MACRA (Medicare Access and CHIP Reauthorization Act of 2015) law.
Category and General Rule Changes for 2021:
Performance Threshold / Payment Adjustment:
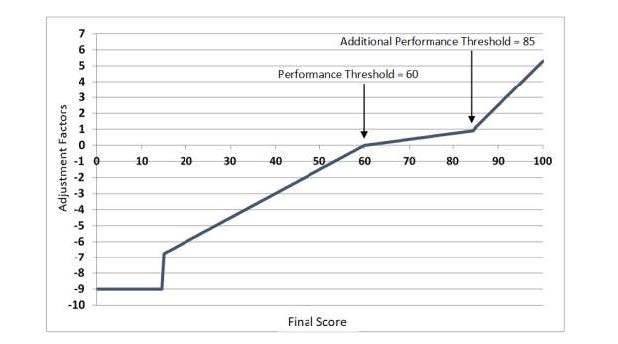
- Payment adjustment for the 2023 payment year remains from - 9% to + (9% x scaling factor) as required by law. (The scaling factor is determined in a way so that budget neutrality is achieved).
- The average expected payment increase is estimated to be 1.4%.
- The maximum bonus is estimated by CMS to be 6.89% for clinicians that reach a MIPS score of 100 on 2021 MIPS reporting. Below one can see an ilustrative example of MIPS Payment Adjustment Factors based on Final Scores and Performance Threshold and Additional Performance Threshold for the 2023 MIPS Payment Year.
- The 2020 payment adjustments (2018 MIPS) varied between -5% and 1.68%.
-
2018 MIPS Points 2020 MIPS Payment Adjustment 0 -5% 3 (Performance threshold) 0% 10 0.02% 20 0.05% 30 0.08% 40 0.11% 50 0.13% 60 0.16% 70 (Exceptional performance threshold) 0.29% 80 0.82% 90 1.35% 100 1.68% 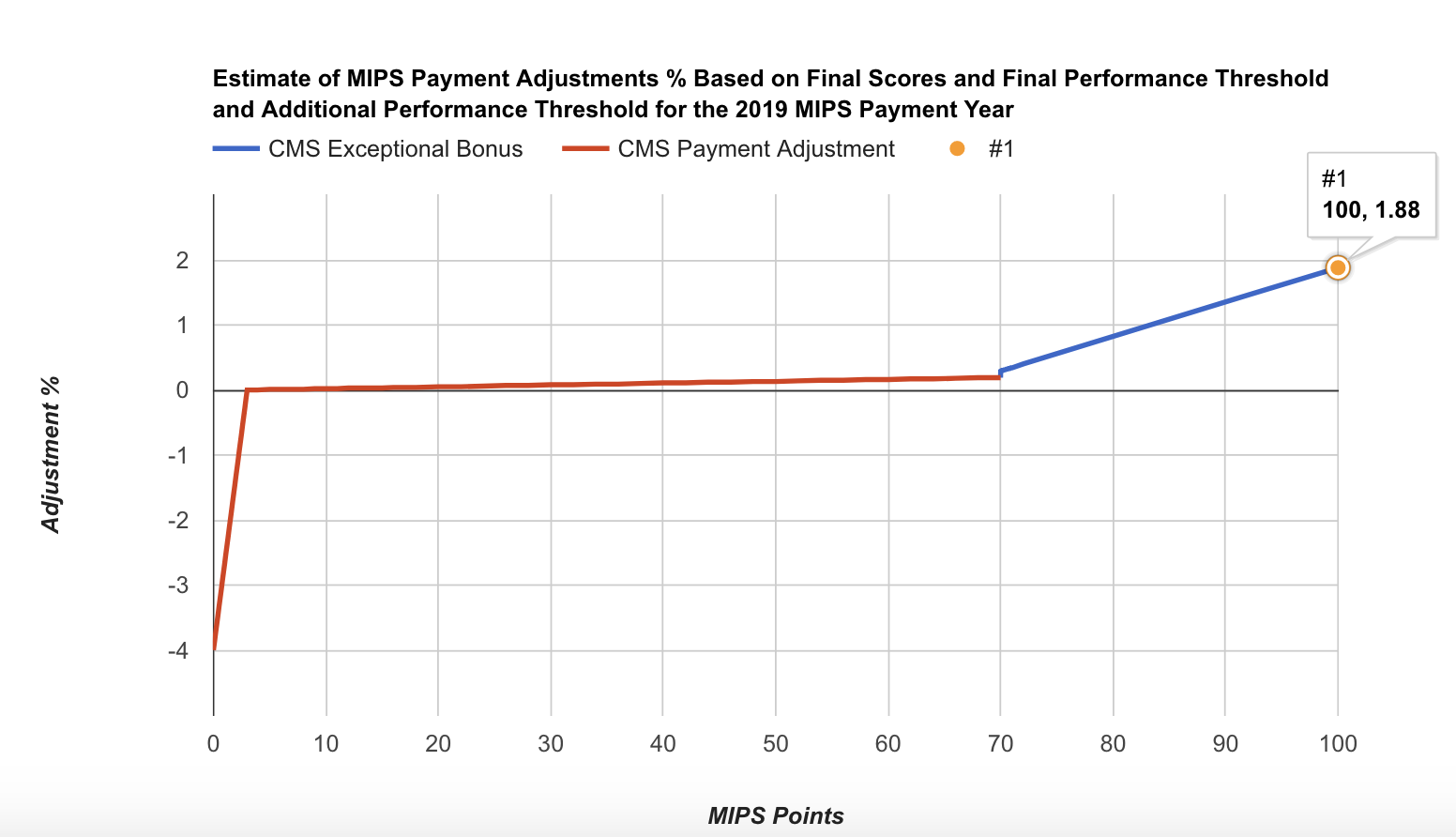
- Performance threshold increases to 60 points for 2021 MIPS (up from 45 points in 2020).
- Additional performance threshold remains 85 points for exceptional performance for 2021 MIPS
- In the 2023 MIPS payment year, MIPS payment adjustments, which only apply to covered professional services (and does not includes Part B drugs), will be applied based on MIPS eligible clinicians’ performance on specified measures and activities within four integrated performance categories.
- CMS estimates that MIPS payment adjustments will be approximately equally distributed between negative MIPS payment adjustments ($433 million) and positive MIPS payment adjustments ($433 million) to MIPS eligible clinicians, as required by the statute to ensure budget neutrality.
- Positive MIPS payment adjustments will also include up to an additional $500 million for exceptional performance to MIPS eligible clinicians whose final score meets or exceeds the exceptional performance threshold of 85 points.
- CMS estimates that 92.5% of MIPS eligible clinicians that participate in MIPS are expected to receive positive or neutral payment adjustments.
- The final MIPS payment adjustments will be determined by the distribution of final scores across MIPS eligible clinicians and the performance threshold:
- More MIPS eligible clinicians above the performance threshold means the scaling factors would decrease because more MIPS eligible clinicians receive a positive MIPS payment adjustment factor.
- More MIPS eligible clinicians below the performance threshold means the scaling factors would increase because more MIPS eligible clinicians would receive a negative MIPS payment adjustment factor and relatively fewer MIPS eligible clinicians would receive a positive MIPS payment adjustment factor.
MIPS Eligibility:
- Eligible clinician types remain the same as 2020.
- CMS would maintain a single MIPS determination period that would be used for purposes of the low-volume threshold and to identify MIPS eligible clinicians as non-patient facing, a small practice, hospital-based, and ASC-based, as applicable:
- An initial 12-month segment beginning on October 1, 2019 to September 30, 2020; and
- A second 12-month segment beginning on October 1, 2020 to September 30, 2021.
- If a TIN or TIN/NPI did not exist in the first segment, but does exist in the second segment, these eligible clinicians could be eligible for MIPS. For example, the eligible clinician may not find their TIN or TIN/NPI in the QPP lookup tool, but may still be eligible if they exceed the low-volume threshold in the second segment.
- No Change in the Low-Volume Threshold (LVT):
- To be excluded from MIPS, clinicians or groups would need to meet one of the following three critera:
- Have ≤ $90K in Part B allowed charges for covered professional services,
- Provide care to ≤ 200 Part B enrolled beneficiaries, OR
- Provide ≤ 200 covered professional services under the Physician Fee Schedule (PFS)
- To be excluded from MIPS, clinicians or groups would need to meet one of the following three critera:
- Virtual Group participation continues, which is another way clinicians can elect to participate in MIPS.
- MIPS Opt-in:
- Clinicians or groups will be able to opt-in to MIPS again in 2021 if they meet or exceed at least 1, but not all three, of the low-volume threshold criterion.
- Individual clinicians and groups could make an election to opt-in or voluntarily report MIPS via the Quality Payment Program portal by logging into their account and selecting either the option to opt-in (positive, neutral, or negative MIPS adjustment) or to remain excluded and voluntarily report (no MIPS adjustment).
- Clinicians and groups opting-in to participate in MIPS would be considered MIPS eligible clinicians, and therefore subject to the MIPS payment adjustment factor. Once the clinician or group elects to opt-in to MIPS, the decision is irrevocable and cannot be changed for the applicable performance period.
- Clinicians who do not decide to opt-in to MIPS would remain excluded and may choose to voluntarily report. Such clinicians would not receive a MIPS payment adjustment factor.
Performance Categories and Performance Period:
- Quality: 12-month calendar year performance period.
- Cost: 12-month calendar year performance period.
- Promoting Interoperability: 90 days minimum performance period.
- Improvement Activities: 90 days minimum performance period.
Quality:
- Weight to final score: 40% (reduced from 45% in 2020).
- Report 6 measures, including one Outcome or other High Priority measure for 12 months on at least 70% of eligible encounters to possibly earn more than 3 points on a measure. Note: Small practices (less than 16 in the practice) can earn 3 points on a measure if at least 1 eligible case is reported.
- Data completeness: completeness threshold is 70% of eligible cases over the entire year, regardless of payer.
- Scoring: Maintains 3-point floor for measures scored against a benchmark. Maintains 3 points for measures that don’t have a benchmark or don’t meet case minimum requirement. Measures that do not meet data completeness requirements will get 0 points instead of 1 point, except that small practices (15 or less in the TIN) will continue to get 3 points.
- Small practices would still receive a 6 point bonus added to the Quality performance score.
- For the 2020 performance period only: CMS is doubling the complex patient bonus so that clinicians, groups and APM Entities can earn up to 10 bonus points (instead of 5 bonus points) to account for the additional complexity of treating their patient population due to COVID-19.
- Improvement Scoring for Quality: Improvement scoring continues to be based on the rate of improvement so that higher improvement will result in more points. Improvement is measured at the Quality performance category level. Up to 10 percentage points available in the Quality performance category.
- High Priority Bonus Points Remain the Same (after first required measure):
- 2 points for outcome, patient experience;
- 1 point for other high priority measures which need to meet data completeness, case minimum, and have performance greater than 0;
- Capped bonus points at 10% of the denominator of total Quality performance category;
- No high priority measure bonus points for CMS Web Interface reporters.
- There are no changes to collection types, submitter types or submission types.
- Collection type is a set of quality measures with comparable specifications and data completeness criteria, including, as applicable:
- eCQMs;
- MIPS Clinical Quality Measures (MIPS CQMs);
- QCDR measures;
- Medicare Part B claims measures;
- CMS Web Interface measures;
- CAHPS for MIPS survey;
- Administrative claims measures.
- Submitter type is the MIPS eligible clinician, group, or third party intermediary acting on behalf of a MIPS eligible clinician or group, as applicable, that submits data on measures and activities under MIPS.
- Submission type is the mechanism by which a submitter type submits data to CMS, including, as applicable:
- Direct: allows users to transmit data through a computer-to-computer interaction, such as an API.
- Log in and upload: allows users to upload and submit data in the form and manner specified by CMS with a set of authenticated credentials.
- Log in and attest: allows users to manually attest that certain measures and activities were performed in the form and manner specified by CMS with a set of authenticated credentials.
- Medicare Part B claims: only available to MIPS eligible clinicians in small practices (15 or fewer in the TIN).
- CMS Web Interface.
- Collection type is a set of quality measures with comparable specifications and data completeness criteria, including, as applicable:
Data Submission Types for MIPS Eligible Clinicians Reporting as Individuals:
|
Performance Category/Submission Combinations Accepted |
Submission Type | Submitter Type |
Collection Type |
|---|---|---|---|
| Quality |
Direct Log in and upload Medicare Part B claims (small practices) |
Individual or Third Party Intermediary Individual |
eCQMs MIPS CQMs QCDR measures Medicare Part B claims measures (small practices) |
|
Cost |
No data submission required | Individual | - |
|
Promoting Interoperability |
Direct Log in and upload Log in and attest |
Individual or Third Party Intermediary | - |
|
Improvement Activities |
Direct Log in and upload Log in and attest |
Individual or Third Party Intermediary | - |
Data Submission Types for MIPS Eligible Clinicians Reporting as Groups:
|
Performance Category/Submission Combinations Accepted |
Submission Type | Submitter Type |
Collection Type |
|---|---|---|---|
| Quality |
Direct Log in and upload CMS Web Interface (groups of 25 or more eligible clinicians) Medicare Part B claims (small practices) |
Group or Third Party Intermediary
|
eCQMs MIPS CQMs QCDR measures CMS Web Interface measures Medicare Part B claims measures (small practices) CMS approved survey vendor measure Administrative claims measures |
|
Cost |
No data submission required | Group | - |
|
Promoting Interoperability |
Direct Log in and upload Log in and attest |
Group or Third Party Intermediary | - |
|
Improvement Activities |
Direct Log in and upload Log in and attest |
Group or Third Party Intermediary | - |
- In 2021, individual eligible clinicians can again submit a single measure via multiple collection types (e.g. MIPS CQM, eCQM, QCDR measures and Medicare Part B claims measures) and be scored on the data submission with the greatest number of measure achievement points.
- Topped out measures: final determination of which measure benchmarks are subject to the topped out cap would not be available until the 2020 MIPS Quality Benchmarks’ file is released.
- CMS will establish flat percentage benchmarks for limited cases where CMS determines that the measure’s benchmark could potentially incentivize inappropriate treatment for some patients.
- CMS is revising the scoring for measures with specification or coding changes during the performance year. In these cases, for each measure that is submitted and impacted by significant changes, performance is based on data for 9 consecutive months of the performance period. If data is not available or may result in patient harm or misleading results, the measure is suppressed.
- New quality measures:
- #479 Hospital-Wide, 30-Day, All-Cause Unplanned Readmission (HWR) Rate for the Merit-Based Incentive Payment System (MIPS) Groups - (Collection type = Administrative Claims)
- #480 Risk-standardized complication rate (RSCR) following elective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA) for Merit-based Incentive Payment System - (Collection type = Administrative Claims)
- #478 Functional Status Change for Patients with Neck Impairments (MIPS CQM)
- Measures removed for 2021 reporting:
- #069: Hematology: Multiple Myeloma: Treatment with Bisphosphonates
- #146: Radiology: Inappropriate Use of “Probably Benign” Assessment Category in Screening Mammograms
- #333: Adult Sinusitis: Computerized Tomography (CT) for Acute Sinusitis (Overuse)
- #348: Implantable Cardioverter-Defibrillator (ICD) Complications Rate
- #390: Hepatitis C: Discussion and Shared Decision Making Surrounding Treatment Options
- #408: Opioid Therapy Follow-up Evaluation
- #412: Documentation of Signed Opioid Treatment Agreement
- #414: Evaluation or Interview for Risk of Opioid Misuse
- #435: Quality of Life Assessment for Patients With Primary Headache Disorders
- #437: Rate of Surgical Conversion from Lower Extremity Endovascular Revascularization Procedure
- #458: All-Cause Hospital Readmission (submitted via claims)
- Qualty Measures added to or removed from existing Specialty Measure Sets:
- Allergy and Immunology - 4 measures added:
- #331: Adult Sinusitis: Antibiotic Prescribed for Acute Viral Sinusitis (Overuse)
- #332: Adult Sinusitis: Appropriate Choice of Antibiotic: Amoxicillin With or Without Clavulanate Prescribed for Patients with Acute Bacterial Sinusitis (Appropriate Use)
- #398: Optimal Asthma Control
- #444: Medication Management for People with Asthma
- Cardiology - 2 measures added:
- #110: Preventive Care and Screening: Influenza Immunization
- #111: Pneumococcal Vaccination Status for Older Adults
- Electrophysiology Cardiac Specialist- 1 measure removed:
- #348: Implantable Cardioverter- Defibrillator (ICD) Complications Rate
- Clinical Social Work - 1 measure added:
- #47: Advance Care Plan
- Diagnostic Radiology - 1 measure removed:
- #146: Radiology: Inappropriate Use of “Probably Benign” Assessment Category in Screening Mammograms
- Emergency Medicine - 1 measure added/ 1 removed:
- Added: #418: Osteoporosis Management in Women Who Had a Fracture
- Removed: #333: Adult Sinusitis: Computerized Tomography (CT) for Acute Sinusitis (Overuse)
- Endocrinology - 2 measures added:
- #110: Preventive Care and Screening: Influenza Immunization
- #111: Pneumococcal Vaccination Status for Older Adults
- Family Medicine - 4 measures removed:
- #333: Adult Sinusitis: Computerized Tomography (CT) for Acute Sinusitis (Overuse)
- #408: Opioid Therapy Follow-up Evaluation
- #412: Documentation of Signed Opioid Treatment Agreement
- #414: Evaluation or Interview for Risk of Opioid Misuse
- Gastroenterology - 1 measure removed:
- #390: Hepatitis C: Discussion and Shared Decision Making Surrounding Treatment Options
- Geriatrics - 2 measures removed:
- #412: Documentation of Signed Opioid Treatment Agreement
- #414: Evaluation or Interview for Risk of Opioid Misuse
- Internal Medicine - 2 measures added, 4 measures removed:
- Added:
- #107 (eCQM): Adult Major Depressive Disorder (MDD): Suicide Risk Assessment
- #391: Follow-Up After Hospitalization for Mental Illness (FUH)
- Removed:
- #333: Adult Sinusitis: Computerized Tomography (CT) for Acute Sinusitis (Overuse)
- #408: Opioid Therapy Follow-up Evaluation
- #412: Documentation of Signed Opioid Treatment Agreement
- #414: Evaluation or Interview for Risk of Opioid Misuse
- Added:
- Interventional Radiology - 1 measure removed:
- #437: Rate of Surgical Conversion from Lower Extremity Endovascular Revascularization Procedure
- Neurology - 2 measures added, 4 measure removed:
- Added:
- #277: Sleep Apnea: Severity Assessment at Initial Diagnosis
- #279: Sleep Apnea: Assessment of Adherence to Positive Airway Pressure Therapy
- Removed:
- #408: Opioid Therapy Follow-up Evaluation
- #412: Documentation of Signed Opioid Treatment Agreement
- #414: Evaluation or Interview for Risk of Opioid Misuse
- #435: Quality Of Life Assessment For Patients With Primary Headache Disorders
- Added:
- Neurosurgical - 2 measures added:
- #260: Rate of Carotid Endarterectomy (CEA) for Asymptomatic Patients, without Major Complications (Discharged to Home by Post- Operative Day #2)
- #344: Rate of Carotid Artery Stenting (CAS) for Asymptomatic Patients, Without Major Complications (Discharged to Home by Post- Operative Day #2)
- Oncology/Hematology - 1 measure removed:
- #069: Hematology: Multiple Myeloma: Treatment with Bisphosphonates
- Ophthalmology - 1 measure added:
- #238: Use of High-Risk Medications in Older Adults
- Orthopedic Surgery - 3 measures removed:
- #408: Opioid Therapy Follow-up Evaluation
- #412: Documentation of Signed Opioid Treatment Agreement
- #414: Evaluation or Interview for Risk of Opioid Misuse
- Otolaryngology - 1 measure removed:
- #333: Adult Sinusitis: Computerized Tomography (CT) for Acute Sinusitis (Overuse)
- Pediatrics - 1 measure added:
- #116: Avoidance of Antibiotic Treatment for Acute Bronchitis/Bronchiolitis
- Physical Medicine - 3 measures removed:
- #408: Opioid Therapy Follow-up Evaluation
- #412: Documentation of Signed Opioid Treatment Agreemen
- #414: Evaluation or Interview for Risk of Opioid Misuse
- Physical Therapy/Occupational Therapy - 2 measures added, 1 measure removed:
- Added:
- #283 Dementia Associated Behavioral and Psychiatric Symptoms Screening and Management
- #286 Dementia: Safety Concern Screening and Follow-Up for Patients with Dementia
- Removed:
- #282 Dementia: Functional Status Assessment
- Added:
- Pulmonology - 2 measures added:
- #110: Preventive Care and Screening: Influenza Immunization
- #111: Pneumococcal Vaccination Status for Older Adults
- Skilled Nursing - 2 measures added:
- #111: Pneumococcal Vaccination Status for Older Adults
- #238: Use of High-Risk Medications in Older Adults
- Speech Language Pathology - 1 measure added:
- #134: Preventive Care and Screening: Screening for Depression and Follow-Up Plan
- Thoracic Surgery - 1 measure added:
- #44: Coronary Artery Bypass Graft (CABG): Preoperative Beta- Blocker in Patients with Isolated CABG Surgery
- Urgent Care - 1 measure removed:
- #333: Adult Sinusitis: Computerized Tomography (CT) for Acute Sinusitis (Overuse)
- Allergy and Immunology - 4 measures added:
Improvement Activities:
- Weight to final score: 15%
- No change in the number of activities that MIPS eligible clinicians have to report to reach a total of 40 points. MIPS eligible clinicians in small practices and practices in a rural areas will keep reporting on no more than 2 medium or 1 high-weighted activity to reach the highest score. Large practices attest to either 2 high weighted, 4 medium weighted or 1 high and 2 medium weighted activities for full credit in this category.
- CMS is modifying two previously adopted improvement activities in the Inventory, removing one previously adopted improvement activity, and finalizing one improvement activity that was originally adopted in the March 31st COVID-19 IFC (85 FR 19277) and continued with modification in the September 2nd COVID-19 IFC (85 FR 54850 through 54851).
- For group reporting, the participation threshold is 50% of the clinicians in the practice. At least 50% of a group’s NPIs must perform the same activity for the same continuous 90 days in the performance period.
- Rural area is changed to mean a ZIP code designated as rural by the Federal Office of Rural Health Policy (FORHP) using the most recent FORHP Eligible ZIP Code file available.
- Modified Improvement Activities:
- lA_BE_4 Engagement of patient through implementation of improvements in patient portal (Medium-weighted)
- The modification would add language to include caregivers as additional potential users of the patient portal, instead of just patients and clinicians, given the important role caregivers can play in bidirectional information exchange regarding the clinical care of the patient
- The modification would also add language to clarify that the portal’s use should be for “bidirectional information exchange between the patient and their provider” and “the primary use...should be clinical, and not administrative.”
- lA-AHE-7 Comprehensive Eye Exams (Medium-weighted)
- The modification would add language that expands the types of services that eligible clinicians can promote to underserved and/or high-risk populations to receive credit for this activity.
- lA_BE_4 Engagement of patient through implementation of improvements in patient portal (Medium-weighted)
- Improvement Activities Proposed for Removal:
- lA CC 5 CMS Partner in Patients Hospital Engagement Network (Medium-weighted)
- Covid Improvement Activity Finalized:
- IA_ERP_3 COVID-19 Clinical Data Reporting with or without Clinical Trial (High-weighted)
- Expand this improvement activity to include clinicians participating in the care of a patient diagnosed with COVID-19 who simultaneously submit their clinical patient data to a clinical data registry for research. Commenters noted that this expansion will increase clinician participation in this improvement activity and increase the availability of COVID-19 patient data.
- IA_ERP_3 COVID-19 Clinical Data Reporting with or without Clinical Trial (High-weighted)
Promoting Interoperability:
- Weight to final score: 25%
- MIPS eligible clinicians must continue to use 2015 Edition certified EHR technology to report this category.
- Maintains small set of objectives:
- e-Prescribing:
- e-prescribing
- Query of Prescription Drug Monitoring Program (PDMP)
- Health Information Exchange:
- Support Electronic Referral Loops By Sending Health Information Measure
- Support Electronic Referral Loops By Receiving and Reconciling Health Information
- Provider to Patient Exchange:
- Provide Patients Electronic Access to Their Health Information
- Public Health and Clinical Data Exchange (choose 2)
- Immunization Registry Reporting,
- Electronic Case Reporting,
- Public Health Registry Reporting,
- Clinical Data Registry Reporting,
- Syndromic Surveillance Reporting)
- e-Prescribing:
- A group will be identified as hospital-based and eligible for reweighting if more than 75% of the NPIs in the group meet the definition of a hospital-based individual MIPS eligible clinician.
- CMS will reweight the Promoting Interoperability performance category to 0 and reallocate the performance category weight of 25% to the Quality performance category for the following reasons:
- Automatic reweighting:
- Hospital-based MIPS eligible clinicians;
- Non-Patient Facing clinicians;
- Ambulatory Surgical Center (ASC)— based MIPS eligible clinicians, finalized retroactive to the transition year;
- Nurse practitioners, physician assistants, clinical nurse specialist, certified registered nurse anesthetists;
- Reweighting extends to additional clinician types (physical therapists, occupational therapists, speech-language pathologists, audiologists, clinical psychologists and registered dietitians and nutrition professionals).
- Continues reweighting policy through an approved hardship application.
- Automatic reweighting:
Cost:
- Weight to final score: 20% (up from 15% in 2020)
- CMS will maintain the existing Cost measures:
- TPCC measure
- MSPB Clinician measure (no change from CY2020)
- 18 existing episode-based cost measures
- CMS added telehealth services directly applicable to existing episode-based cost measures and the TPCC measure.
- Case minimum of 10 for procedural episodes and 20 for acute inpatient medical condition episodes.
- CMS will calculate cost measure performance; no action is required from clinicians.
MIPS APM Reporting Options
- MIPS eligible clinicians in APMs would be given the option to participate in MIPS and submit data at the individual, group, or APM Entity level. The APM Scoring Standard (reporting requirements and scoring approach for APM participants) will end beginning with the 2021 performance period. CMS is also eliminating APM Entity level low-volume threshold determinations. Instead, MIPS eligibility will be determined only at the individual or group level.
New Alternative Payment Model (APM) Performance Pathway
The APM Performance Pathway (APP) is created to streamline reporting for APMs and will begin for the 2021 performance year. This new pathway is designed to align with the MVP when it is implemented. Features of the APP include:
- The Quality performance category will be weighted at 50% of the MIPS Final Score.
- A fixed set of quality measures (APP Core Quality Measure Set):
- #1 Diabetes: Hemoglobin A1c (HbA1c) Poor Control
- #134 Preventive Care and Screening: Screening for Depression and Follow-up Plan
- #236 Controlling High Blood Pressure
- #321 CAHPS for MIPS Survey
- Hospital-Wide, 30-day, All-Cause Unplanned Readmission (HWR)
- Rate Risk Standardized, All-Cause Unplanned Admissions for Multiple Chronic Conditions for ACOs
- The Cost performance category will be weighted at 0%.
- The Improvement Activity (IA) performance category will be weighted at 20%. The score will automatically be assigned based on the IA requirements of the MIPS APM in which the MIPS eligible clinician participates. All APM participants would earn an automatic score of 100% on the IA performance category for the 2021 performance period.
- The Promoting Interoperability performance category will be weighted at 30%.
- QCDRs, Qualified Registries, and Health IT Vendors could support data submission for the program.
- Note: The CMS Web Interface will be an optional, alternative collection type for a subset of quality measures in the APP for the 2021 performance period only.
MIPS Value Pathways (MVPs) beginning in 2022
-
CMS will delay the adoption of the MIPS Value Pathway (MVP) framework until the 2022 performance period or later. The MVP framework is intended to align and connect measures and activities across the Quality, Cost, Promoting Interoperability, and Improvement Activities performance categories of MIPS for different specialties or condition.
-
CMS created some illustrative diagrams regarding the MIPS Value Pathways: