2023 MIPS Performance Feedback and Final Score
If you submitted 2023 Merit-based Incentive Payment System (MIPS) data, you can now view your performance feedback and MIPS final score on the Quality Payment Program website.
Your final performance feedback includes your MIPS Final Score and the Total Payment Adjustment that will apply after January 1, 2025.
The 2024 MIPS payment adjustments vary between -9% and +8.25%. A perfect score of 100 MIPS points would result in a positive payment adjustment of +8.25%.
The 2023 MIPS payment adjustments varied between -9% and +2.33%.
For comparison, the 2021 MIPS payment adjustments varied between -9% and +1.87%.
How will MIPS payment adjustments be reflected on remittance advice (RA) documents?
If a MIPS payment adjustment is applied to a payment made to a MIPS eligible clinician, the following codes will be displayed on the RA:
|
Positive MIPS Payment Adjustments |
CARC 144: "Incentive adjustment, e.g. preferred product/service" | RARC N807: "Payment adjustment based on the Merit-based Incentive Payment System (MIPS)." |
Group Code: CO. This group code is used when a contractual agreement between the payer and payee, or a regulatory requirement, resulted in an adjustment. |
|
Negative MIPS Payment Adjustments |
CARC 237: "Legislated/Regulatory Penalty. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.)" | RARC N807: "Payment adjustment based on the Merit-based Incentive Payment System (MIPS)." |
Group Code: CO |
Overview: Final Score and Payment Adjustment
How is my final score determined?
Your final score is the sum of your performance category scores and any additional bonus points (e.g., your complex patient bonus). Scroll down the Overview page to the Additional Awarded Bonus Points section for a breakdown of these bonus points.
How does my payment adjustment relate to my final score?
The MIPS Adjustment is broken into 2 parts - Payment Adjustment and Exceptional Performance Adjustment for a total adjustment. Payment adjustments are determined on a sliding scale based on your final score.
*The 2022 performance year/2024 payment year is the last year for the additional MIPS payment adjustment for exceptional performance. |
Application of Performance Year MIPS Final Scoring to New TINs in Payment Year
If a doctor has a new Taxpayer Identification Number (TIN) and National Provider Identification (NPI) combination, CMS will use the NPI's MIPS Final Score from the previous TIN to determine the doctor's payment adjustment. If the doctor has multiple scores from different TINs, CMS will use the highest score.
Quality
I submitted more than 6 measures. How did CMS determine which ones counted towards my Quality performance category score?
If you submitted more than 6 measures, only 6 of those measures will contribute points to your Quality performance category score. However, CMS will include any bonus points from the remaining measures, as long as you haven’t exceeded the 10% cap for the applicable bonus.
CMS first selected your highest scored outcome measure, or another high priority measure if there were no outcome measures submitted. CMS then selected the next 5 highest scored measures. When there are multiple measures with the same score, CMS selects measures for the top six based on (ascending) numerical order of the measure ID. If you didn’t submit an outcome or other high priority measure, you will only see 5 measures that counted towards the category score and a score of 0 out of 10 for the 6th required measure unless the Eligible Measure Applicability process determined that none were available to you.
Why don’t I see Improvement Scoring in my Total Quality Score calculation?
Just as with other aspects of feedback, CMS only displays the data that’s relevant to you. You will only see an Improvement Score if you qualified for it.
How is the Improvement Score calculated?
Improvement scoring is calculated by comparing the Quality performance category achievement percent score from the previous period to the Quality performance category achievement percent score in the current period. Measure bonus points are not included in improvement scoring.
Example: In 2018, a MIPS eligible clinician earned 25 measure achievement points and 2 measure bonus points for reporting an additional outcome measure. For the 2019 performance period, the same MIPS eligible clinician earned 33 measure achievement points and 6 measure bonus points for end-to-end electronic reporting.
- 2018 Quality performance category achievement percent score =
- 42% (25/60)
- Excludes the 2 bonus points
- 2019 Quality performance category achievement percent score =
- 55% o (33/60)
- Excludes the 6 bonus points
- The increase in Quality performance category achievement percent score from prior performance period to current performance period =
- 13% o (55% - 42%)
- The improvement percent score is 3.1% which will be added to the percent score earned for reported measures.
- (13%/42%)*10% = 3.1%
- Please note that the improvement percent score cannot be negative and is capped at 10%.
Why are measures with higher performance rates not counted towards my Quality performance category score?
CMS included your highest scoring quality measures. Remember that scoring is determined by comparing the performance rate to the measure’s benchmark. If you submit two measures, each with an 85% performance rate, one may earn 7 points while the other earns 10 points, based on the benchmarks for each measure.
I submitted all of the Medicare Part B claims measures (or MIPS CQMs, “registry” measures) available to me. How do I know if the Eligible Measure Applicability (EMA) process was applied to my submission?
Your feedback will indicate whether your submission qualified for a denominator (“Total Possible Points”) reduction through the EMA process. 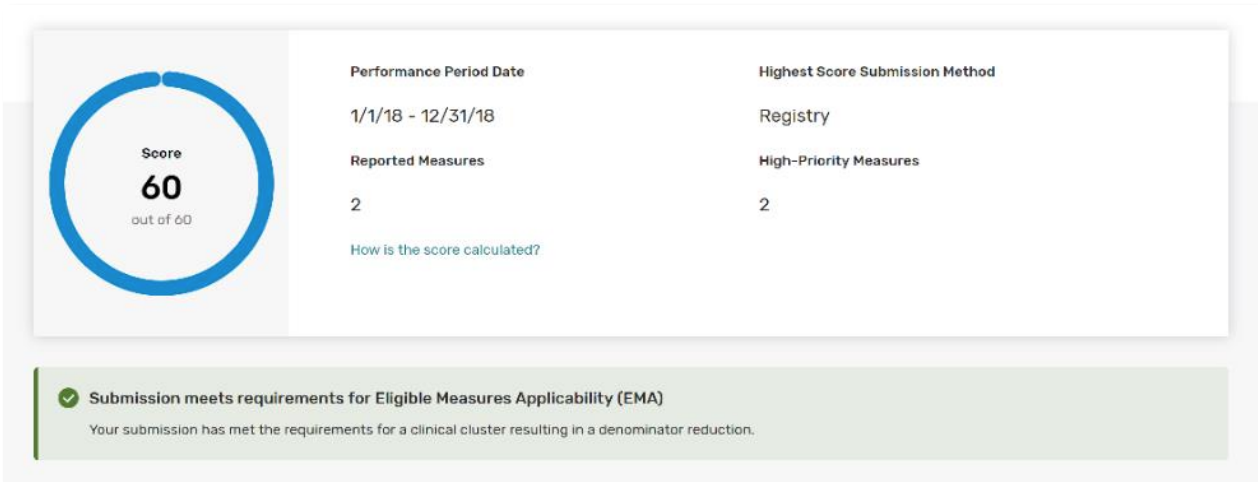
In the screenshot below, the Quality score calculations show a reduced denominator of 40 points, meaning there were 4 required measures.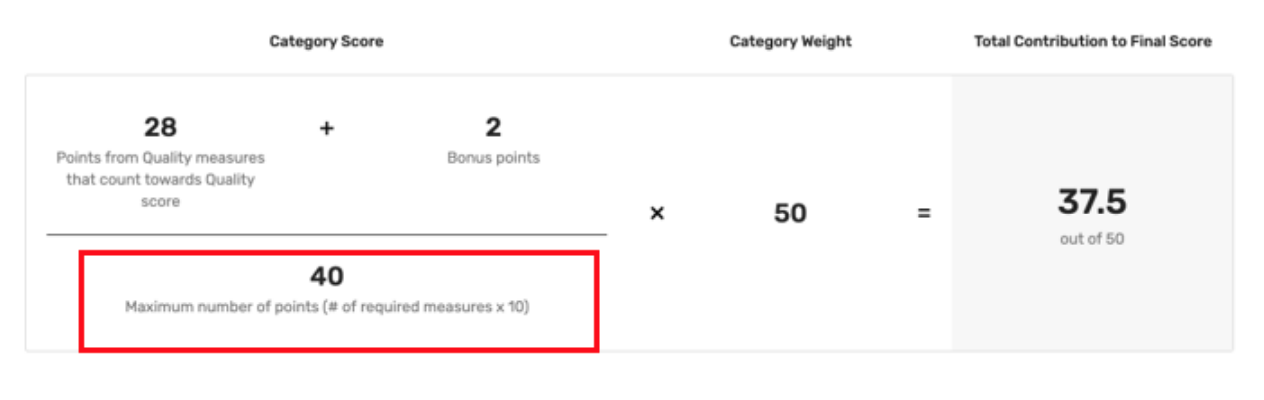
In the screenshot below, the Quality score calculations show a standard denominator of 60 points, meaning that you were accountable for submitting 6 measures.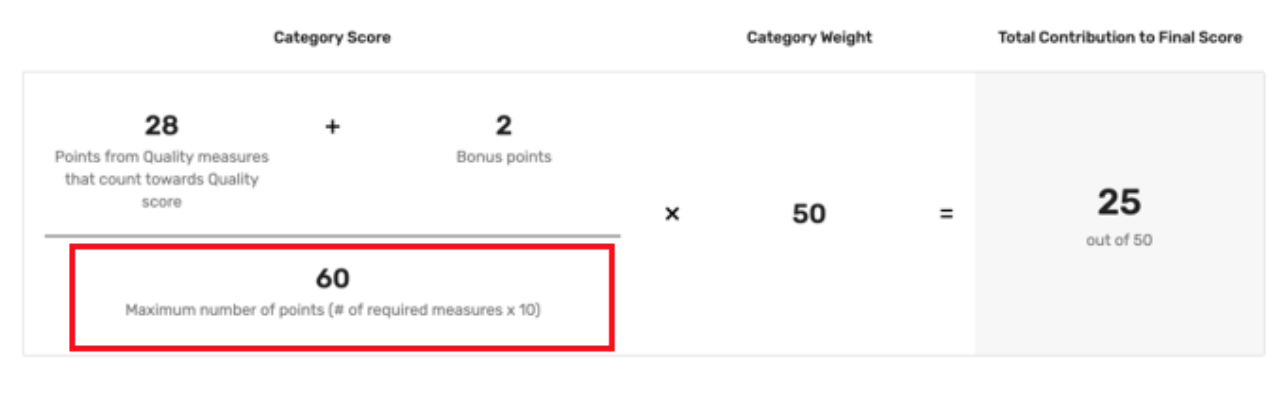
If you submitted all available measures through claims or Registry and were still scored out of 60 Total Possible Points (or 70 if you participated as a group and were scored on the All-Cause Hospital Readmission measure), you may want to request a targeted review so CMS can take another look.
Improvement Activities
We are a certified patient-centered medical home. Why didn’t we receive full credit in the Improvement Activities performance category?
You are required to attest during the submission period to being a certified/ recognized patient-centered medical home to earn this credit.
f you’re a MIPS eligible clinician practicing in a certified patient-centered medical home, including Medical Homes Model, or a comparable specialty practice, you’ll earn full credit for the Improvement Activities performance category as long as you attested to this during the submission period.
Promoting Interoperability
Why did I receive a performance category score of 0 out of 25 points when I qualified for reweighting?
If a MIPS eligible clinician or group submitted any data for the performance category in which they were intending to be reweighted, CMS scored them according to the data submitted and the category was NOT reweighted to 0%.
If you did not submit data and received a performance category score of 0 but should have qualified for reweighting based on your clinician type, special status, and/or hardship status, you may need to request a targeted review.
Cost
Why don’t I see any cost measure information?
CMS is reweighting the cost performance category from 20% to 0% for the 2021 performance period for all MIPS eligible clinicians, regardless of participation as an individual, group, virtual group or APM Entity. The 20% cost performance category weight will be redistributed to other performance categories.
Items and Services
What is the purpose of the Items and Services section of MIPS performance feedback?
The Items and Services section of your performance feedback includes information about your patients’ health care utilization and emergency department use. The purpose of this breakdown is to provide clinicians and groups with additional information on the types of Medicare covered items and used by their patients throughout a calendar year. Please note that the Items and Services data is for informational purposes only and will not affect your MIPS performance scores.
How is CMS defining the types of Items and Services used by patients?
CMS defines the types of items and services utilized by patients using Healthcare Common Procedure Coding System (HCPCS) codes. The HCPCS codes represent a standard coding system for procedures, supplies, products and services billed by health care providers. The data in the Items and Services section of performance feedback is aggregated by ranges of HCPCS codes for ease of review.
What if there’s an error with my Payment Adjustment/Performance Feedback/Final Score?
If you believe an error has been made in your 2022 MIPS payment adjustment calculation, you can request a targeted review until October 1st, 2021 at 8:00 pm (Eastern). However, CMS encourages you to request a targeted review as soon as possible if you identify an error with your MIPS final performance feedback and MIPS payment adjustment factor(s) to help ensure that the correct payment adjustment is applied to your claims from the start of the 2023 payment year.
What is a Targeted Review?
A targeted review is a process where MIPS eligible clinicians or groups can request that CMS review the calculation of their 2023 MIPS payment adjustment factor and, as applicable, their additional MIPS payment adjustment factor for exceptional performance.
Examples of Reasons for Targeted Review
- I submitted all of the quality measures available to me but my denominator wasn’t reduced.
- My data was submitted under the wrong TIN or NPI.
- I have a special status that isn’t reflected in my performance category scoring.
- I was scored in “x” performance category but was approved for reweighting through an exception application (Extreme and Uncontrollable Circumstances Application/ Promoting Interoperability Hardship Application).
- I was identified as a QP but I’m not a participant in an Advanced APM.
- I’m a participant in a MIPS APM but I didn’t receive a final score associated with my APM Entity.
- I work on a small practice who was automatically scored as a group on Medicare Part B claims quality measures.
How Do I Request a Targeted Review?
Step 1. You may request a targeted review by signing into your QPP account here.
Step 2. Select Targeted Review from the left-hand navigation page.
Step 3. Add New Targeted Review to access the Targeted Review Application.
Step 4. Select Application Type that aligns with how you submitted your 2021 MIPS data (e.g., Individual, Group, etc.) and then provide requested identifying information.
Step 5. Enter Submission Information - Individual, Group, Virtual Group, APM Entity Details.
Step 6. Select Performance Categories that were affected by the issue(s) you experienced.
Step 7. Select Issue Type and attach supporting documentation.
Step 8. Certify and Submit for Review.
You can also request a targeted review on the Quality Payment Program website. More information about the targeted review process can be found in this CMS guide.
Why Would a Clinician Request a Targeted Review?
The following are examples of circumstances under which a MIPS eligible clinician or group may wish to request a targeted review:
- A MIPS eligible clinician or group submitted performance data under the incorrect Tax Identification Number (TIN) or National Provider Identifier (NPI).
- A MIPS eligible clinician or group has supporting documentation indicating that certain errors were made, such as eligibility being wrongly assigned to the MIPS eligible clinician or group (e.g. the MIPS eligible clinician or group fell below the low-volume threshold and should not have received a payment adjustment).
- A MIPS eligible clinician has supporting documentation indicating that they should qualify for automatic reweighting of performance categories due to the 2021 policy for extreme and uncontrollable circumstances.
- A MIPS eligible clinician has supporting documentation indicating that they were erroneously excluded from the APM participation list and should have been scored under the APM scoring standard.
- Please note that this is not a comprehensive list of circumstances. CMS encourages all MIPS participants to submit a request if, after reviewing final performance feedback, they can provide supporting documentation that a targeted review of their MIPS payment adjustment factor (or additional MIPS payment adjustment factor) is warranted.
When Can I Request Targeted Review?
Requests for a targeted review can be submitted immediately following the release of the 2021 performance feedback.
Requests can be submitted now until October 21, 2022, at 8:00pm EST but CMS strongly encourages everyone to submit a request as soon as possible. This will help to ensure payment adjustments are applied correctly from the start of the payment year.
When evaluating a targeted review request, CMS may require documentation to support the request. If the targeted review request is approved, CMS may update the final score and/or associated payment adjustment (if applicable), as soon as technically feasible. Please note that targeted review decisions are final and not eligible for further review.
Allow MDinteractive to access and review your MIPS performance feedback and payment adjustment information?
To allow MDinteractive to review your MIPS reports and send you feedback, please log in to your MDinteractive account and click on the QPP Performance Feedback button.