On November 1, 2024, the Centers for Medicare & Medicaid Services (CMS) released the 2025 Medicare Physician Fee Schedule (PFS) Final Rule. This rule outlines updates to the Quality Payment Program (QPP), including key changes to the Merit-based Incentive Payment System (MIPS), Alternative Payment Models (APMs), and related reporting requirements for the 2025 performance year. Below is a summary of key policy updates from 2024, along with all major requirements for the 2025 MIPS performance period affecting eligible clinicians and groups.
MIPS Eligibility & Participation Overview
What’s New for 2025?
There are no changes to MIPS eligibility criteria or participation options for the 2025 performance year.
Who is Eligible?
Clinicians are required to participate in MIPS if they:
- Belong to a MIPS-eligible clinician type
- Exceed all three elements of the low-volume threshold during both segments of the MIPS Determination Period:
- Bill more than $90,000 in Medicare Part B allowed charges for covered professional services; and
- Provide covered professional services to more than 200 Medicare Part B beneficiaries; and
- Furnish more than 200 covered professional services to Medicare Part B beneficiaries.
Determination Periods
CMS assesses eligibility using two 12-month segments:
- Segment 1: October 1, 2023 – September 30, 2024
- Segment 2: October 1, 2024 – September 30, 2025
Exemptions
Clinicians are excluded from MIPS if they:
- Are newly enrolled in Medicare during the performance period.
- Participate sufficiently in an Advanced Alternative Payment Model (APM) and are designated as Qualifying APM Participants (QPs).
- Do not exceed the low-volume threshold in either segment of the determination period.
How to Check Your Eligibility
Your initial 2025 MIPS eligibility status is available now. CMS will publish your final eligibility status in December 2025. If you work at multiple practices, you may be required to report at one but not at another—eligibility is determined at the TIN/NPI level.
- Use the QPP Participation Status Tool
Reporting Options
There are several ways to participate in MIPS for the 2025 performance year. Choose the option that best fits your practice:
Traditional MIPS
Traditional MIPS is the original reporting pathway. Below is a summary of what is required for each performance category:
- Quality - Select 6 measures (including an Outcome or High Priority measure) and collect data for the full year (Jan 1–Dec 31). Review the quality measure benchmarks when selecting measures to understand how benchmarks affect scoring. You may also choose to report a complete specialty measure set as an alternative to selecting individual measures. In addition, CMS will automatically evaluate any applicable claims-based measures.
- Improvement Activities - Choose 2 activities and perform each for at least 90 continuous days. Some clinicians with special status have reduced requirements.
- Promoting Interoperability measures - Report the complete measure set for a continuous 180-day period. Some clinicians with special status may not be required to report data for this performance category.
- Cost - No data submission required. CMS calculates your Cost performance category score based on claims.
MIPS Value Pathways (MVPs)
MVPs are a newer, more streamlined option tailored to specific specialties or conditions. Each MVP includes a focused set of:
- Quality measures - Select 4 measures within the MVP and collect data for the full year (Jan 1–Dec 31). CMS also evaluates a population health measure using claims data.
- Improvement Activities - Choose 1 activity within the MVP and perform it for at least 90 continuous days.
- Promoting Interoperability - Report the measure set for a continuous 180-day period. Some clinicians with special status may not be required to report data for this performance category.
- Cost measures - No data submission required. CMS scores you using MVP-specific cost measures.
MIPS APM Participants
The Alternative Payment Model (APM) Performance Pathway (APP) is a simplified reporting framework available to clinicians participating in a MIPS APM. It features a defined set of quality measures and is designed to reduce reporting burden, provide additional scoring opportunities, and promote greater participation in APMs.
Performance Threshold Remains at 75 Points
For the 2025 performance period, the MIPS performance threshold will remain at 75 points. Each clinician’s or group’s performance across the MIPS categories will be combined into a Final Score ranging from 0 to 100 points. This score is then compared to the 75-point threshold to determine whether a positive, neutral, or negative payment adjustment will apply. Payment adjustments based on 2025 performance will continue to range up to ±9%.
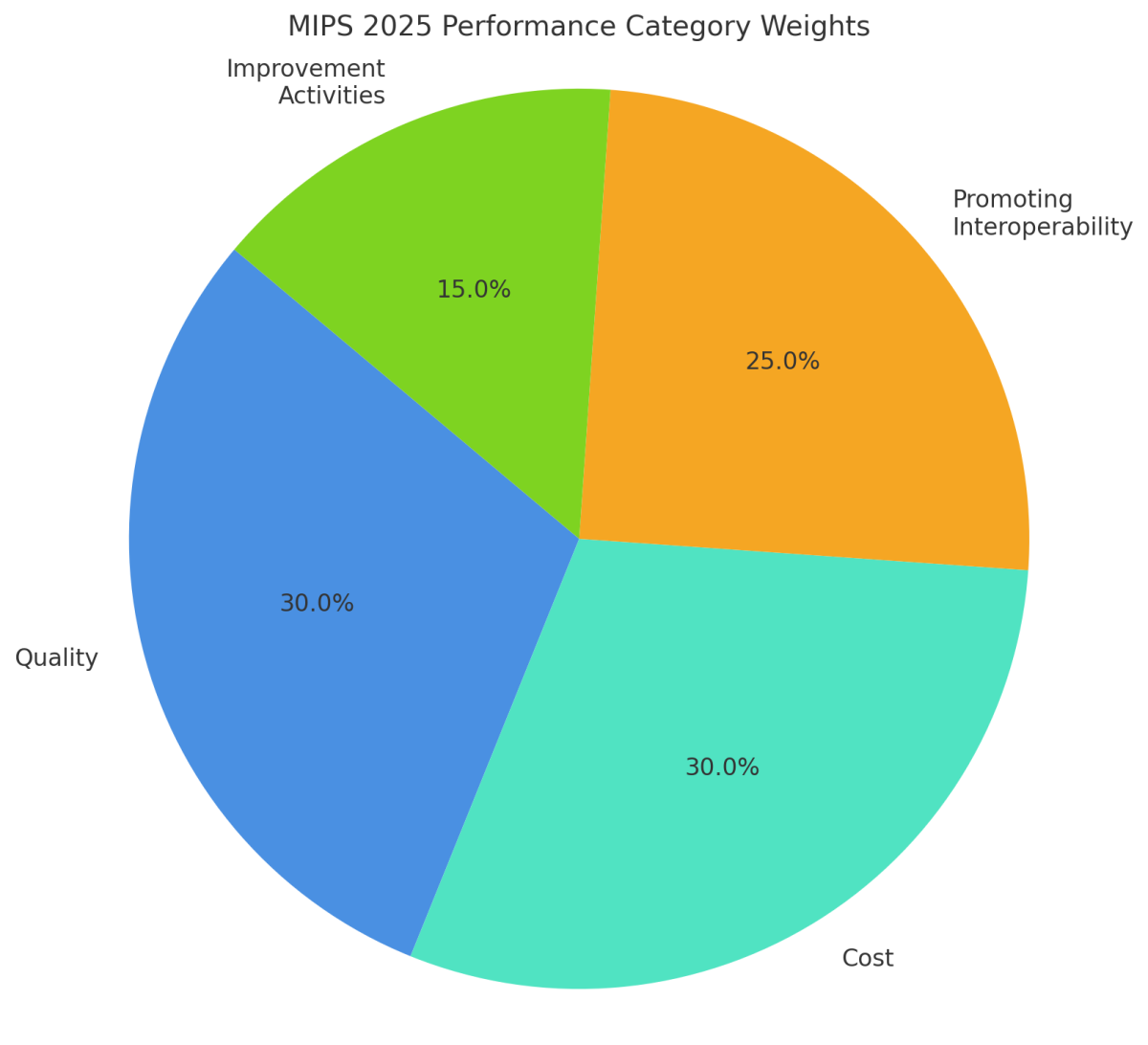
2025 Performance Category Weights
Understanding how each MIPS performance category contributes to your final score is essential for successful reporting in 2025. The chart below shows the percentage weight assigned to each category.
Small practices automatically receive reweighting for the Promoting Interoperability (PI) category. If a small practice does not submit PI data, the Quality category will be weighted at 40% and Improvement Activities at 30%.
MIPS Performance Category Weight Redistribution Policies
Depending on your practice size and reporting circumstances, CMS may reweight one or more performance categories. The tables below outline how performance category weights are adjusted for both large and small practices in 2025.
Large Practice Participants
The table below illustrates the 2025 performance category reweighting policies that CMS will apply to large practice participants (practice has 16 or more clinicians):
| Reweighting Scenario | Quality | Cost | Improvement Activities (IA) | Promoting Interoperability (PI) |
|---|---|---|---|---|
| No Reweighting Needed | ||||
| Scores for all 4 performance categories | 30% | 30% | 15% | 25% |
| Reweight 1 Performance Category | ||||
| No Cost | 55% | 0% | 15% | 30% |
| No PI | 55% | 30% | 15% | 0% |
| No Quality | 0% | 30% | 15% | 55% |
| No IA | 45% | 30% | 0% | 25% |
| Reweight 2 Performance Categories | ||||
| No Cost and no PI | 85% | 0% | 15% | 0% |
| No Cost and no Quality | 0% | 0% | 15% | 85% |
| No Cost and no IA | 70% | 0% | 0% | 30% |
| No PI and no Quality | 0% | 50% | 50% | 0% |
| No PI and no IA | 70% | 30% | 0% | 0% |
| No Quality and no IA | 0% | 30% | 0% | 70% |
Small Practice Participants
The table below illustrates the 2025 performance category reweighting policies that CMS will apply to small practice participants (practice has 15 or fewer clinicians):
| Reweighting Scenario | Quality | Cost | Improvement Activities (IA) | Promoting Interoperability (PI) |
|---|---|---|---|---|
| No Reweighting Needed | ||||
| Scores for all 4 performance categories | 30% | 30% | 15% | 25% |
| Reweight 1 Performance Category | ||||
| No Cost | 55% | 0% | 15% | 30% |
| No PI* | 40% | 30% | 30% | 0% |
| No Quality | 0% | 30% | 15% | 55% |
| No IA | 45% | 30% | 0% | 25% |
| Reweight 2 Performance Categories | ||||
| No Cost and no PI* | 50% | 0% | 50% | 0% |
| No Cost and no Quality | 0% | 0% | 15% | 85% |
| No Cost and no IA | 70% | 0% | 0% | 30% |
| No PI and no Quality | 0% | 50% | 50% | 0% |
| No PI and no IA | 70% | 30% | 0% | 0% |
| No Quality and no IA | 0% | 30% | 0% | 70% |
Quality Measure Inventory Changes
There are a total of 195 quality measures for the 2025 performance period which reflect:
- 6 new Quality measures
- 1 quality measure was finalized for addition in the calendar year (CY) 2024 Medicare Physician Fee Schedule (PFS) Final Rule for the CY 2025 MIPS performance period
- Removal of 9 Quality measures
- Substantive changes to 66 existing Quality measures
A list of new measures, along with their collection types, is outlined in the table below.
*In the CY 2024 PFS Final Rule, measure Q494: Excessive Radiation Dose or Inadequate Image Quality for Diagnostic Computed Tomography (CT) in Adults (Clinician Level), was finalized with a 1-year delay to the CY 2025 performance period.
A list of measures that have been removed or partially removed is outlined in the table below.
| Retired Quality Measures | Collection Type |
|---|---|
| #019: Diabetic Retinopathy: Communication with the Physician Managing Ongoing Diabetic Care | MIPS CQM |
| #104: Prostate Cancer: Combination Androgen Deprivation Therapy for High Risk or Very High Risk Prostate Cancer | MIPS CQM |
| #137 Melanoma: Continuity of Care – Recall System: Oncology: Medical and Radiation – Plan of Care for Pain | MIPS CQM |
| #254 Ultrasound Determination of Pregnancy Location for Pregnant Patients with Abdominal Pain | MIPS CQM |
| #260 Rate of Carotid Endarterectomy (CEA) for Asymptomatic Patients, without Major Complications (Discharged to Home by Post-Operative Day #2) | MIPS CQM |
| #409 Clinical Outcome Post Endovascular Stroke Treatment | MIPS CQM |
| #433 Proportion of Patients Sustaining a Bowel Injury at the time of any Pelvic Organ Prolapse Repair | MIPS CQM |
| #436: Radiation Consideration for Adult CT: Utilization of Dose Lowering Techniques* | MIPS CQM |
| #439 Age Appropriate Screening Colonoscopy | MIPS CQM |
| #452 Patients with Metastatic Colorectal Cancer and RAS (KRAS or NRAS) Gene Mutation Spared Treatment with Antiepidermal Growth Factor Receptor (EGFR) Monoclonal Antibodies | MIPS CQM |
| #472 Appropriate Use of DXA Scans in Women Under 65 Years Who Do Not Meet the Risk Factor Profile for Osteoporotic Fracture | eCQM |
*Measure #436: Radiation Consideration for Adult CT: Utilization of Dose Lowering Techniques was already finalized for removal with a 1-year delay to the CY 2025 performance period.
Quality Measure Benchmarks
When clinicians or groups submit measures for the quality performance category, their performance on each measure is compared against the measure's benchmark to determine how many points the measure earns. A clinician or group can receive anywhere from 1 to 10 points for each MIPS measure based on this comparison as long as the data completeness standards and case minimum requirements are met. When selecting measures to report, carefully review the 2025 benchmarks to understand how measures will be scored.
Flat Benchmarks for a Subset of Topped-Out Measures
A flat benchmarking methodology will be used for certain topped-out measures, specifically those within specialty sets that have limited options and a high number of topped-out measures, where there is a lack of new measure development. This approach aims to address challenges in meaningful MIPS participation in these areas. Each year, CMS will propose the specific measures to which this policy will apply and detail the corresponding benchmarks.
| Performance Rate | Available Points |
|---|---|
| 84-85.9% | 1-1.9 |
| 86-87.9% | 2- 2.9 |
| 88-89.9% | 3-3.9 |
| 90-91.9% | 4-4.9 |
| 92-93.9% | 5-5.9 |
| 94-95.9% | 6-6.9 |
| 96-97.9% | 7-7.9 |
| 98-99.9% | 8-8.9 |
| 99-99.99% | 9-9.9 |
| 100% | 10 |
Improvement Activities Category Updates
Improvement Activities Inventory
A total of 104 Improvement Activities are available for the 2025 performance period. Updates to the Improvement Activities inventory reflect the following changes:
- Two new activities
- Modification of 1 existing activity
- Removal of 4 activities
| New Improvement Activities | Retired Improvement Activities |
|---|---|
| IA_PM_24 Implementation of Protocols and Provision of Resources to Increase Lung Cancer Screening Uptake | EPA_1 Provide 24/7 Access to MIPS Eligible Clinicians or Groups Who Have Real-Time Access to Patient's Medical Record |
| IA_PM_25 Save a Million Hearts: Standardization of Approach to Screening and Treatment for Cardiovascular Disease Risk | ERP_4 Implementation of a Personal Protective Equipment (PPE) Plan |
| ERP_5 Implementation of a Laboratory Preparedness Plan | |
| PSPA_27 Invasive Procedure or Surgery Anticoagulation Medication Management |
Improvement Activities: 2025 Scoring and Reporting Updates
Beginning with the 2025 performance year, CMS is simplifying Improvement Activity (IA) reporting by removing activity weightings. This change reduces the number of activities clinicians need to attest to in order to earn full credit in this performance category.
Reporting Requirements by Participation Type
Traditional MIPS Reporting
Clinicians, groups, and virtual groups with any of the following special statuses:
- Small Practice
- Rural
- Non–Patient Facing
- Health Professional Shortage Area (HPSA)
→ Must attest to one improvement activity.
All other clinicians, groups, and virtual groups:
→ Must attest to two improvement activities.
MIPS Value Pathways (MVP) Reporting
All clinicians, groups, and subgroups (regardless of special status):
→Must attest to one improvement activity.
Promoting Interoperability (PI) Category Updates
There are no major changes to the Promoting Interoperability performance category for the 2025 performance year.
However, beginning with the 2025 performance period (impacting the 2027 MIPS payment year), clinical social workers will no longer qualify for automatic reweighting. This exemption applied only through the 2024 performance year.
Automatic reweighting will continue to apply only to MIPS eligible clinicians, groups, and virtual groups with the following special statuses:
- Ambulatory Surgical Center (ASC)-based
- Hospital-based
- Non–Patient Facing
- Small Practice
Cost Category Updates
CMS is introducing six new episode-based cost measures and updating two existing ones. These measures will apply at both the group (TIN) and individual clinician (TIN/NPI) levels. To be scored, clinicians must meet a minimum of 20 episodes per measure.
New Episode-Based Cost Measures
- Acute Inpatient Medical Condition:
- Respiratory Infection Hospitalization
- Chronic Condition Measures:
- Chronic Kidney Disease
- End-Stage Renal Disease
- Kidney Transplant Management
- Prostate Cancer
- Rheumatoid Arthritis
Updated Episode-Based Cost Measures
- Cataract Removal with Intraocular Lens (IOL) Implantation (formerly Routine Cataract with IOL Implantation)
- Inpatient Percutaneous Coronary Intervention (PCI) (formerly ST-Elevation Myocardial Infarction [STEMI] PCI)
Cost Measure Scoring: New Exclusion Policy
Beginning with the 2024 performance period (impacting the 2026 MIPS payment year), CMS will implement a revised cost measure exclusion policy to better align with policies in other performance categories.
Key updates include:
- Expanded reasons for exclusion:
Cost measures may now be excluded due to either:
→ Significant changes, or
→ Errors in measure design or calculation.
- Timing flexibility:
Exclusions may apply even if the issue occurs outside of the performance period, as long as it impacts performance within that period.
Cost Measure Benchmarking: Methodology Changes
Updates to the cost measure benchmarking methodology take effect with the 2024 performance period and the 2026 MIPS payment year.
Key features of the revised approach:
- Median alignment: The median cost will correspond to the performance threshold for that year. For example, in 2024, the median score is set at 7.5, matching the 75-point threshold.
- Standard deviation-based ranges: Scoring ranges will be defined using standard deviations from the median, providing a more statistically driven benchmarking structure.
These changes will be reflected when final MIPS scores are issued in summer 2025.
MIPS Value Pathways (MVPs)
There are 21 MVPs available for 2025. This includes six new MVPs:
- Complete Ophthalmologic Care MVP
- Dermatological Care MVP
- Gastroenterology Care MVP
- Optimal Care for Patients with Urological Conditions MVP
- Pulmonology Care MVP
- Surgical Care MVP
The Optimal Care for Patients with Episodic Neurological Conditions and the Supportive Care for Neurodegenerative Conditions MVPs have been combined into a single consolidated neurological MVP titled Quality Care for Patients with Neurological Conditions.
A full list of 2025 MVPs can be found here.
Population Health Measure Changes
MVP participants will no longer select a population health measure during registration. Instead, CMS will calculate all available measures and apply the highest scoring one to the participant’s quality score.
Advanced Primary Care Management Service Codes and MVP Reporting
Starting January 1, 2025, physicians and non-physician practitioners, such as nurse practitioners, physician assistants, and clinical nurse specialists, can bill for Advanced Primary Care Management (APCM) services if they provide comprehensive primary care, serve as the main coordinator of a patient’s healthcare, and obtain verbal or written consent from the patient. These services are intended for primary care specialties such as internal medicine, family medicine, geriatrics, and pediatrics.
To support this model, CMS introduced three new APCM billing codes (G0556, G0557, G0558) that bundle chronic care services into a monthly payment and eliminate time-based billing requirements. However, beginning with the 2025 performance year, clinicians using these codes must report through the Value in Primary Care MIPS Value Pathway (MVP). Practices not participating in an Accountable Care Organization must register for this MVP and meet all required reporting criteria within the MVP to avoid denied APCM claims and a potential 9% payment penalty on Medicare Part B reimbursements.
Complex Organization Adjustment
APM entities, including Medicare Shared Savings Program (MSSP) Accountable Care Organizations (ACOs), can earn 1 bonus point per qualifying eCQM, capped at 10% of total quality category points, to support eCQM reporting.
Medicare Shared Savings Program (MSSP) Accountable Care Organizations (ACOs)
Starting in 2025, MSSP ACOs must report using the new APM Performance Pathway (APP) Plus measure set:
- Starts with 6 measures, expanding to 11 by 2028
- Reporting options: eCQMs, MIPS CQMs, or Medicare CQMs
- Flat benchmarks apply to Medicare CQMs for the first two years
- Incentives extended to support eCQM and MIPS CQM adoption
More information regarding the ACO APP reporting requirements can be found here.