Your Final 2025 MIPS Eligibility Is In—Here’s What to Do Next





As clinicians begin planning for the 2025 MIPS performance year, the Improvement Activities (IA) performance category remains a key opportunity to maximize your MIPS score with relatively low effort. The Centers for Medicare and Medicaid Services (CMS) finalized some notable updates to the IA category this year, including a smaller number of required attestations and simplified scoring. This post outlines the key updates for 2025 and shares a practical list of Improvement Activities that are both broadly relevant and commonly used across specialties, making them simple for most practices to implement.
CMS just released its 2023 Quality Payment Program (QPP) Results At a Glance and there’s a lot to unpack, especially for clinicians navigating MIPS, MVPs, and APMs. Whether you’re a solo provider, part of a group, or operating under an APM entity, this report offers important insights that could impact your 2025 Medicare payments. Let’s break down the key takeaways and how MDinteractive can help you turn this knowledge into action.

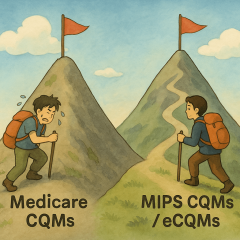
The Merit-based Incentive Payment System (MIPS) continues to evolve, bringing new challenges and opportunities for clinicians aiming to optimize their performance and meet the Centers for Medicare and Medicaid Services (CMS) reporting requirements. As in past years, success with MIPS in 2025 will require a proactive strategy, careful planning, and timely data collection throughout the year. In this article, we’ve outlined a step-by-step checklist to help your practice stay organized, reduce reporting burdens, and achieve success with 2025 MIPS.
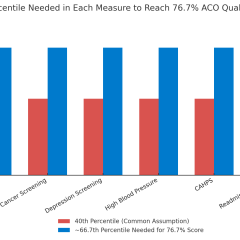
During 2025, all Shared Savings Program ACOs will be required to report the APP Plus quality measure set, which includes four clinical quality measures, the CAHPS survey, and the readmission measure.