On November 1, 2018, CMS released the CY 2019 Quality Payment Program final rule under the MACRA (Medicare Access and CHIP Reauthorization Act of 2015) law. You can find the Fact Sheet here and an Executive Summary here.
Category and General Rule Changes for 2019:
- Performance Threshold / Payment Adjustment:
- Payment adjustment for the 2021 payment year ranges from - 7% to + (7% x scaling factor) as required by law. (The scaling factor is determined in a way so that budget neutrality is achieved.).
- The maximum bonus is estimated by CMS to be 4.69% for clinicians that reach a MIPS score of 100 on 2019 MIPS reporting.
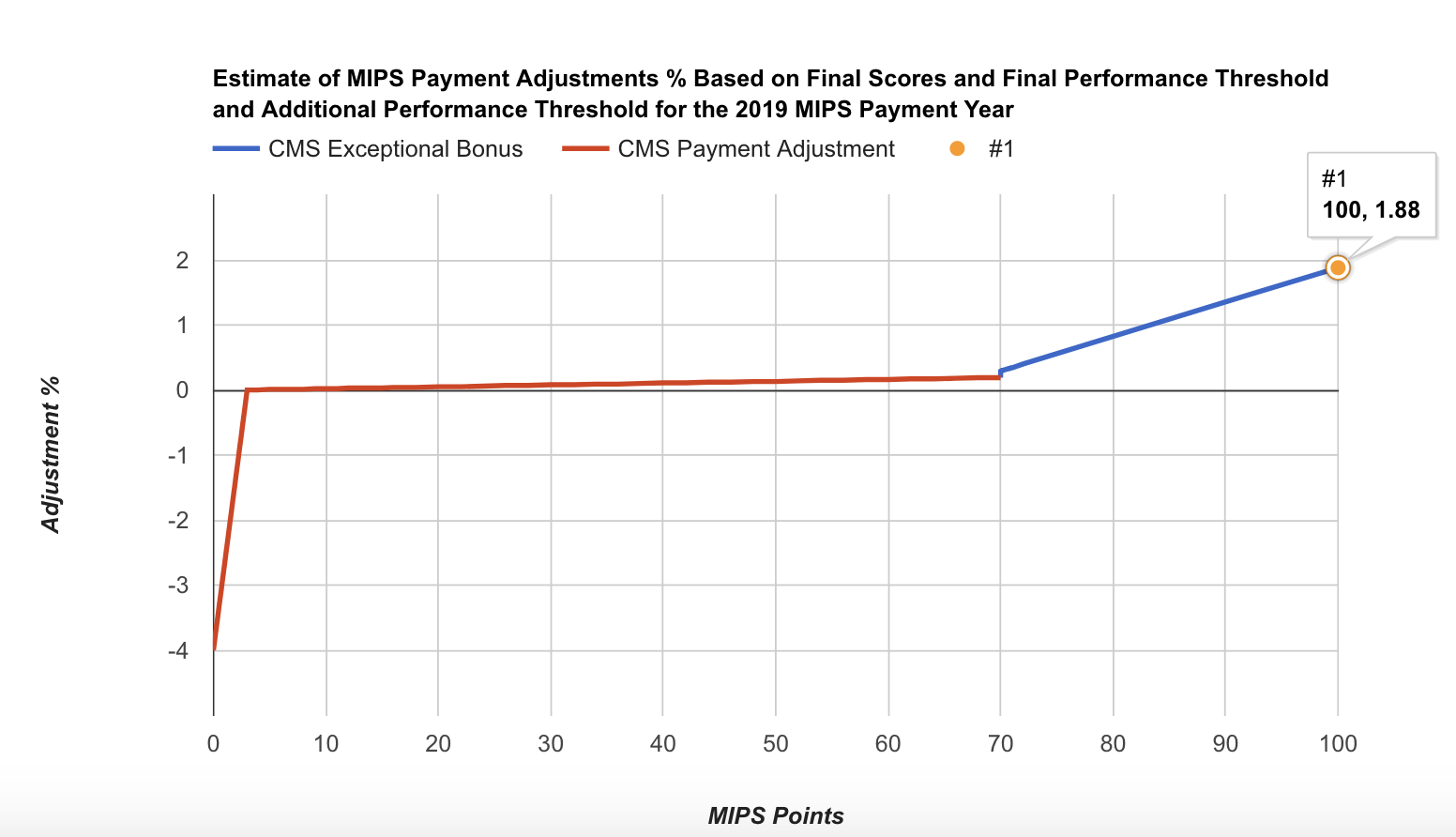
- The scaling factor for the 2019 payment year (2017 MIPS reporting year) was 0.47 (based on MDinteractive's user data). The 2019 payment adjustments varied between -4% and 1.88%. When CMS analyzed the estimated final scores for the 2017 MIPS reporting year, the mean final score was between 63.50 and 68.98 points and the median was between 77.83 and 82.5 points. We estimate that the median positive payment adjustment was ~0.82%:
2017 MIPS Points 2019 MIPS Payment Adjustment 0 -4% 3 (Performance threshold) 0% 10 0.02% 20 0.05% 30 0.08% 40 0.11% 50 0.13% 60 0.16% 70 (Exceptional performance threshold) 0.29% 80 0.82% 90 1.35% 100 1.88% 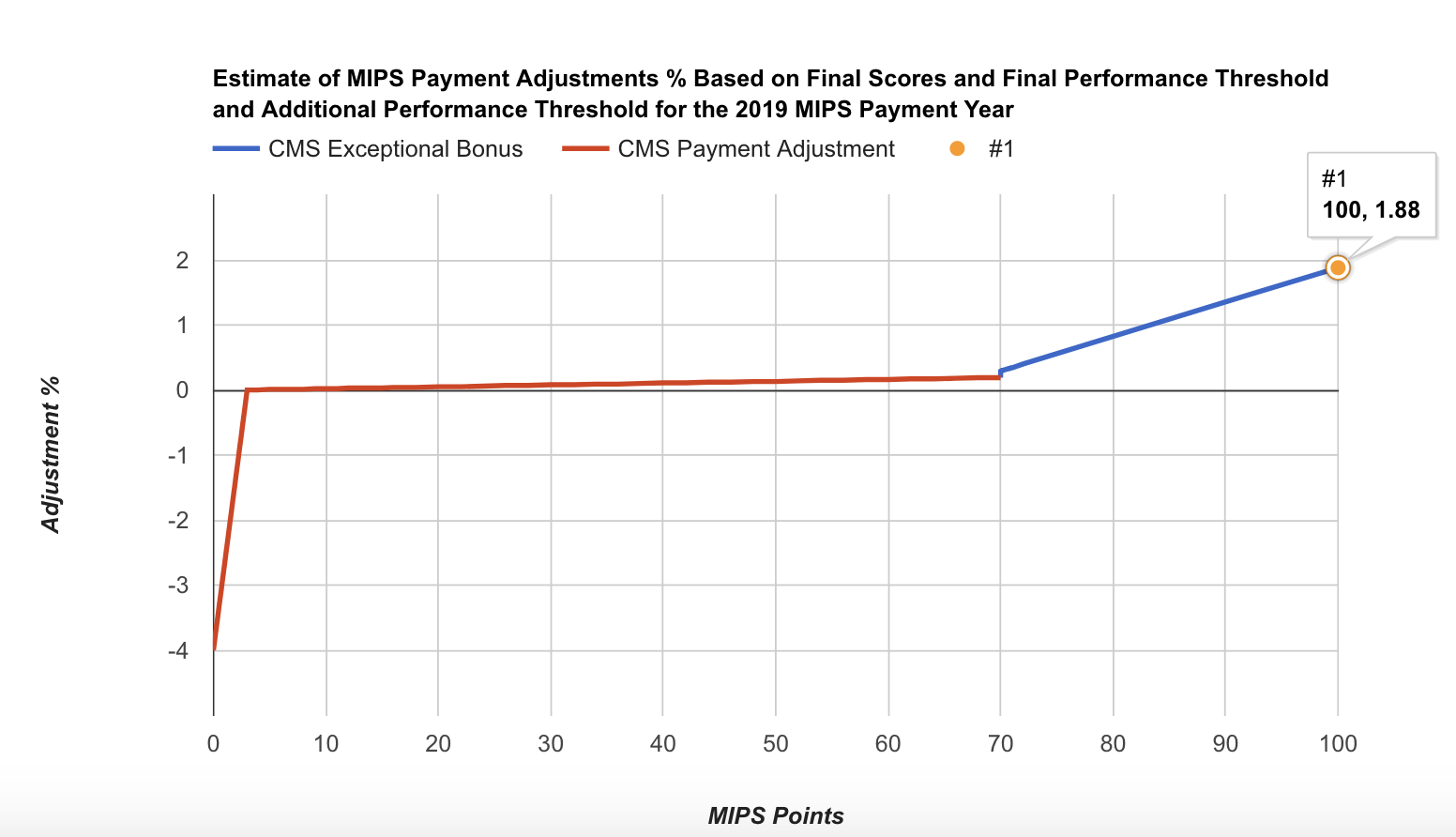
- Performance threshold increases to 30 points for 2019 MIPS (instead of 15 in 2018).
- Additional performance threshold increases to 75 points for exceptional performance for 2019 MIPS.
- In the 2021 MIPS payment year, MIPS payment adjustments, which only apply to covered professional services (and does not includes Part B drugs), will be applied based on MIPS eligible clinicians’ performance on specified measures and activities within four integrated performance categories.
- CMS estimates that MIPS payment adjustments will be approximately equally distributed between negative MIPS payment adjustments ($390 million) and positive MIPS payment adjustments ($390 million) to MIPS eligible clinicians, as required by the statute to ensure budget neutrality.
- Positive MIPS payment adjustments will also include up to an additional $500 million for exceptional performance to MIPS eligible clinicians whose final score meets or exceeds the exceptional performance threshold of 75 points.
- CMS estimates that 91.2% of MIPS eligible clinicians that participate in MIPS are expected to receive positive or neutral payment adjustments.
- The final MIPS payment adjustments will be determined by the distribution of final scores across MIPS eligible clinicians and the performance threshold:
- More MIPS eligible clinicians above the performance threshold means the scaling factors would decrease because more MIPS eligible clinicians receive a positive MIPS payment adjustment factor.
- More MIPS eligible clinicians below the performance threshold means the scaling factors would increase because more MIPS eligible clinicians would receive a negative MIPS payment adjustment factor and relatively fewer MIPS eligible clinicians would receive a positive MIPS payment adjustment factor.
- MIPS Eligibility:
- Eligible clinician types remain the same as 2018 with the following additions:
- Physical therapist
- Occupational therapist
- Clinical psychologist
- Qualified speech-language pathologist
- Qualified audiologist
- Registered dietitian or nutrition professionals
- Eligible clinician types remain the same as 2018 with the following additions:
- CMS creates a single MIPS determination period that would be used for purposes of the low-volume threshold and to identify MIPS eligible clinicians as non-patient facing, a small practice, hospital-based, and ASC-based, as applicable:
- An initial 12-month segment beginning on October 1, 2017 to September 30, 2018; and
- A second 12-month segment beginning on October 1, 2018 to September 30, 2019.
- It is important to note that if a TIN or TIN/NPI did not exist in the first segment, but does exist in the second segment, these eligible clinicians could be eligible for MIPS. For example, the eligible clinician may not find their TIN or TIN/NPI in the Quality Payment Program lookup tool but may still be eligible if they exceed the low-volume threshold in the second segment.
- Low-Volume Threshold (LVT):
- The low-volume threshold will include a third criterion for determining MIPS eligibility. To be excluded from MIPS, clinicians or groups would need to meet one of the following three criterion:
- Have ≤ $90K in Part B allowed charges for covered professional services,
- Provide care to ≤ 200 Part B enrolled beneficiaries, OR
- Provide ≤ 200 covered professional services under the Physician Fee Schedule (PFS)
- The low-volume threshold will include a third criterion for determining MIPS eligibility. To be excluded from MIPS, clinicians or groups would need to meet one of the following three criterion:
- MIPS Opt-in:
- Starting in 2019, clinicians or groups will be able to opt-in to MIPS if they meet or exceed at least 1, but not all three, of the low-volume threshold criterion.
- For individual eligible clinicians and groups to make an election to opt-in or voluntarily report to MIPS, they would make an election via the Quality Payment Program portal by logging into their account and simply selecting either the option to opt-in (positive, neutral, or negative MIPS adjustment) or to remain excluded and voluntarily report (no MIPS adjustment).
- Once the clinician or group elects to opt-in to MIPS, the decision is irrevocable and cannot be changed for the applicable performance period.
- Clinicians who do not decide to opt-in to MIPS would remain excluded and may choose to voluntarily report. Such clinicians would not receive a MIPS payment adjustment factor.
- CMS has developed a website that provides design examples of the different approaches to MIPS participation in CY 2019. The website uses wireframe (schematic) drawings to illustrate the three different approaches to MIPS participation: voluntary reporting to MIPS, opt-in reporting to MIPS, and required to participate in MIPS.
- Individual eligible clinicians and groups opting-in to participate in MIPS would be considered MIPS eligible clinicians, and therefore subject to the MIPS payment adjustment factor. Individual eligible clinicians and groups voluntarily reporting measures and activities for the MIPS are not considered MIPS eligible clinicians, and therefore not subject to the MIPS payment adjustment factor.
- Performance Period:
- Quality: 12-month calendar year performance period.
- Cost: 12-month calendar year performance period.
- Promoting Interoperability: 90 days minimum performance period.
- Improvement Activities: 90 days minimum performance period.
- Quality:
- Weight to final score: 45% (instead of 50% in 2018).
- Data completeness: completeness threshold is 60% (same as 2018) of eligible cases over the entire year, regardless of payer. Measures that do not meet data completeness criteria will get 1 point instead of 3 points. Small practices (15 or less in the TIN) will continue to get 3 points.
- Scoring: Maintains 3-point floor for measures scored against a benchmark. Maintains 3 points for measures that don’t have a benchmark or don’t meet case minimum requirement. Measures that do not meet data completeness requirements will get 1 point instead of 3 points, except that small practices will continue to get 3 points.
- Improvement Scoring for Quality: Improvement scoring will be based on the rate of improvement so that higher improvement will result in more points, particularly for those improving from lower performance in the transition year. Improvement is measured at the Quality performance category level. Up to 10 percentage points available in the Quality performance category.
- Example: In 2018, a MIPS eligible clinician earned 25 measure achievement points and 2 measure bonus points for reporting an additional outcome measure. For the 2019 performance period, the same MIPS eligible clinician earned 33 measure achievement points and 6 measure bonus points for end-to-end electronic reporting.
- 2018 Quality performance category achievement percent score =
- 42% (25/60)
- Excludes the 2 bonus points
- 2019 Quality performance category achievement percent score =
- 55% o (33/60)
- Excludes the 6 bonus points
- The increase in Quality performance category achievement percent score from prior performance period to current performance period =
- 13% o (55% - 42%)
- The improvement percent score is 3.1% which will be added to the percent score earned for reported measures.
- (13%/42%)*10% = 3.1%
- Please note that the improvement percent score cannot be negative and is capped at 10%.
- 2018 Quality performance category achievement percent score =
- Example: In 2018, a MIPS eligible clinician earned 25 measure achievement points and 2 measure bonus points for reporting an additional outcome measure. For the 2019 performance period, the same MIPS eligible clinician earned 33 measure achievement points and 6 measure bonus points for end-to-end electronic reporting.
- High priority measures will include quality measures that relate to opioids.
- High Priority Bonus Points (after first required measure):
- 2 points for outcome, patient experience;
- 1 point for other high priority measures which need to meet data completeness, case minimum, and have performance greater than 0;
- Capped bonus points at 10% of the denominator of total Quality performance category;
- No high priority measure bonus points for CMS Web Interface reporters.
- Collection type is a set of quality measures with comparable specifications and data completeness criteria, including, as applicable:
- eCQMs;
- MIPS Clinical Quality Measures (MIPS CQMs). The term MIPS CQMs would replace what was formerly referred to as registry measures since entities other than registries may submit data on these measures;
- QCDR measures;
- Medicare Part B claims measures;
- CMS Web Interface measures;
- CAHPS for MIPS survey;
- Administrative claims measures.
- Submitter type is the MIPS eligible clinician, group, or third party intermediary acting on behalf of a MIPS eligible clinician or group, as applicable, that submits data on measures and activities under MIPS.
- Submission type is the mechanism by which a submitter type submits data to CMS, including, as applicable:
- Direct: allows users to transmit data through a computer-to-computer interaction, such as an API.
- Log in and upload: allows users to upload and submit data in the form and manner specified by CMS with a set of authenticated credentials.
- Log in and attest: allows users to manually attest that certain measures and activities were performed in the form and manner specified by CMS with a set of authenticated credentials.
- Medicare Part B claims: only available to MIPS eligible clinicians in small practices (15 or fewer in the TIN) beginning in 2019. CMS wants to move away from claims reporting, since approximately 69 percent of the Medicare Part B claims measures are topped out.
- CMS Web Interface.
Data Submission Types for MIPS Eligible Clinicians Reporting as Individuals:
Performance Category/Submission Combinations Accepted | Submission Type | Submitter Type | Collection Type |
|---|---|---|---|
| Quality | Direct Log in and upload Medicare Part B claims (small practices) | Individual or Third Party Intermediary Individual | eCQMs MIPS CQMs QCDR measures Medicare Part B claims measures (small practices) |
Cost | No data submission required | Individual | - |
Promoting Interoperability | Direct Log in and upload Log in and attest | Individual or Third Party Intermediary | - |
Improvement Activities | Direct Log in and upload Log in and attest | Individual or Third Party Intermediary | - |
Data Submission Types for MIPS Eligible Clinicians Reporting as Groups:
Performance Category/Submission Combinations Accepted | Submission Type | Submitter Type | Collection Type |
|---|---|---|---|
| Quality | Direct Log in and upload CMS Web Interface (groups of 25 or more eligible clinicians) Medicare Part B claims (small practices) | Group or Third Party Intermediary
| eCQMs MIPS CQMs QCDR measures CMS Web Interface measures Medicare Part B claims measures (small practices) CMS approved survey vendor measure Administrative claims measures |
Cost | No data submission required | Group | - |
Promoting Interoperability | Direct Log in and upload Log in and attest | Group or Third Party Intermediary | - |
Improvement Activities | Direct Log in and upload Log in and attest | Group or Third Party Intermediary | - |
- In 2019, individual eligible clinicians would be able to submit a single measure via multiple collection types (e.g. MIPS CQM, eCQM, QCDR measures and Medicare Part B claims measures) and be scored on the data submission with the greatest number of measure achievement points.
- Topped out measures: final determination of which measure benchmarks are subject to the topped out cap would not be available until the 2019 MIPS Quality Benchmarks’ file is released in late 2018.
- New quality measures:
- 468 Continuity of Pharmacotherapy for Opioid Use Disorder
- 469 Average Change in Functional Status Following Lumbar Spine Fusion Surgery
- 470 Average Change in Functional Status Following Total Knee Replacement Surgery
- 471 Average Change in Functional Status Following Lumbar Discectomy Laminotomy Surgery
- 472 Appropriate Use of DXA Scans in Women Under 65 Years Who Do Not Meet the Risk Factor Profile for Osteoporotic Fracture
- 473 Average Change in Leg Pain Following Lumbar Spine Fusion Surgery
- 474 Zoster (Shingles) Vaccination
- 475 HIV Screening
- New Urgent Care specialty set of measures:
- #65 Appropriate Treatment for Children with Upper Respiratory Infection (URI)
- #66 Appropriate Testing for Children with Pharyngitis
- #91 Acute Otitis Externa (AOE): Topical Therapy
- #93 Acute Otitis Externa (AOE): Systemic Antimicrobial Therapy – Avoidance of Inappropriate Use
- #116 Avoidance of Antibiotic Treatment in Adults With Acute Bronchitis
- #130 Documentation of Current Medications in the Medical Record
- #131 Pain Assessment and Follow-Up
- #226 Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- #317 Preventive Care and Screening: Screening for High Blood Pressure and Follow-Up Documented
- #331 Adult Sinusitis: Antibiotic Prescribed for Acute Viral Sinusitis (Overuse)
- #332 Adult Sinusitis: Appropriate Choice of Antibiotic: Amoxicillin With or Without Clavulanate Prescribed for Patients with Acute Bacterial Sinusitis (Appropriate Use)
- #333 Adult Sinusitis: Computerized Tomography (CT) for Acute Sinusitis (Overuse)
- #402 Tobacco Use and Help with Quitting Among Adolescents
- #431 Preventive Care and Screening: Unhealthy Alcohol Use: Screening & Brief Counseling
- #464 Otitis Media with Effusion (OME): Systemic AntimicrobialsAvoidance of Inappropriate Use
- New Skilled Nursing Facility specialty set of measures:
- #6 Coronary Artery Disease (CAD): Antiplatelet Therapy
- #7 Coronary Artery Disease (CAD): BetaBlocker Therapy – Prior Myocardial Infarction (MI) or Left Ventricular Systolic Dysfunction (LVEF < 40%)
- #8 Heart Failure (HF): Beta-Blocker Therapy for Left Ventricular Systolic Dysfunction (LVSD)
- #47 Care Plan
- #110 Preventive Care and Screening: Influenza Immunization
- #118 Coronary Artery Disease (CAD): Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor Blocker (ARB) Therapy - Diabetes or Left Ventricular Systolic Dysfunction (LVEF < 40%)
- #154 Falls: Risk Assessment
- #155 Falls: Plan of Care
- #181 Elder Maltreatment Screen and FollowUp Plan
- #317 Preventive Care and Screening: Screening for High Blood Pressure and Follow-Up Documented
- #326 Atrial Fibrillation and Atrial Flutter: Chronic Anticoagulation Therapy
- #474 Zoster (Shingles) Vaccination
- Quality Measures Finalized for Removal:
- #18 Diabetic Retinopathy: Documentation of Presence or Absence of Macular Edema and Level of Severity of Retinopathy
- #43 Coronary Artery Bypass Graft (CABG): Use of Internal Mammary Artery (IMA) in Patients with Isolated CABG Surgery
- #99 Breast Cancer Resection Pathology Reporting: pT Category (Primary Tumor) and pN Category (Regional Lymph Nodes) with Histologic Grade
- #100 Colorectal Cancer Resection Pathology Reporting: pT Category (Primary Tumor) and pN Category (Regional Lymph Nodes) with Histologic Grade
- #122 Adult Kidney Disease: Blood Pressure Management
- #140 Age-Related Macular Degeneration (AMD): Counseling on Antioxidant Supplement
- #156 Oncology: Radiation Dose Limits to Normal Tissues
- #163 Comprehensive Diabetes Care: Foot Exam
- #204 Ischemic Vascular Disease (IVD): Use of Aspirin or Another Antiplatelet
- #224 Melanoma: Overutilization of Imaging Studies in Melanoma
- #251 Quantitative Immunohistochemical (IHC) Evaluation of Human Epidermal Growth Factor Receptor 2 Testing (HER2) for Breast Cancer Patients
- #257 Statin Therapy at Discharge after Lower Extremity Bypass (LEB)
- #263 Preoperative Diagnosis of Breast Cancer
- #276 Sleep Apnea: Assessment of Sleep Symptoms
- #278 Sleep Apnea: Positive Airway Pressure Therapy Prescribed
- #327 Pediatric Kidney Disease: Adequacy of Volume Management
- #334 Adult Sinusitis: More than One Computerized Tomography (CT) Scan Within 90 Days for Chronic Sinusitis (Overuse)
- #359 Optimizing Patient Exposure to Ionizing Radiation: Utilization of a Standardized Nomenclature for Computed Tomography (CT) Imaging
- #363 Optimizing Patient Exposure to Ionizing Radiation: Search for Prior Computed Tomography (CT) Studies Through a Secure, Authorized, Media-Free, Shared Archive
- #367 Bipolar Disorder and Major Depression: Appraisal for alcohol or chemical substance use
- #369 Pregnant women that had HBsAg testing
- #373 Hypertension: Improvement in Blood Pressure
- #423 Perioperative Anti-platelet Therapy for Patients Undergoing Carotid Endarterectomy
- #426 Post-Anesthetic Transfer of Care Measure: Procedure Room to a Post Anesthesia Care Unit (PACU)
- #427 Post-Anesthetic Transfer of Care: Use of Checklist or Protocol for Direct Transfer of Care from Procedure Room to Intensive Care Unit (ICU)
- #447 Chlamydia Screening and Follow-up
- Improvement Activities:
- Weight to final score: 15%
- No change in the number of activities that MIPS eligible clinicians have to report to reach a total of 40 points. CMS is proposing more activities to choose from and changes to existing activities for the Inventory. MIPS eligible clinicians in small practices and practices in a rural areas will keep reporting on no more than 2 medium or 1 high-weighted activity to reach the highest score.
- For group participation, only 1 MIPS eligible clinician in a TIN has to perform the Improvement Activity for the TIN to get credit.
- However, for a group to receive full credit as a certified or recognized patient-centered medical home or comparable specialty practice, at least 50 percent of the practice sites within the TIN must be recognized as a patient-centered medical home or comparable specialty practice
- New Improvement Activities:
- IA_AHE_7 Comprehensive Eye Exams
- IA_BE_ 24 Financial Navigation Program
- IA_BMH_10 Completion of Collaborative Care Management Training Program
- IA_CC_ 18 Relationship-Centered Communication
- IA_PSPA_31 Patient Medication Risk Education
- IA_PSPA_32 Use of CDC Guideline for Clinical Decision Support to Prescribe Opioids for Chronic Pain via Clinical Decision Support
- Promoting Interoperability:
- Weight to final score: 25%
- CMS will require MIPS eligible clinicians to use 2015 Edition certified EHR technology beginning with the 2019 MIPS performance period.
- One of the major improvements of the 2015 Edition is the Application Programming Interface (API) functionality. The API functionality supports health care providers and patient electronic access to health information.
- The 2015 Edition also includes a requirement that products must be able to export data from one patient, a set of patients, or a subset of patients, which is responsive to health care provider feedback that their data is unable to carry over from a previous EHR.
- In the 2015 Edition, the health care provider has the autonomy to export data themselves without intervention by their vendor, resulting in increased interoperability and data exchange in the 2015 Edition.
- CMS is proposing a new scoring methodology, a smaller set of objectives and moving away from the base, performance and bonus score methodology that CMS currently uses:
- Each measure would be scored based on the MIPS eligible clinician’s performance for that measure, based on the submission of a numerator and denominator, except for the measures associated with the Public Health and Clinical Data Exchange objective, which require “yes or no” submissions.
- Each measure would contribute to the MIPS eligible clinician’s total Promoting Interoperability performance category score.
- The scores for each of the individual measures would be added together to calculate the Promoting Interoperability performance category score of up to 100 possible points for each MIPS eligible clinician.
- In general, the Promoting Interoperability performance category score makes up 25 percent of the MIPS final score.
- If a MIPS eligible clinician fails to report on a required measure or claim an exclusion for a required measure if applicable, the clinician would receive a total score of zero for the Promoting Interoperability performance category.
- Security Risk Analysis remains part of the requirements for the Promoting Interoperability performance category, but would no longer be scored as a measure.
- Smaller set of objectives:
- e-Prescribing:
- e-prescribing (10 points)
- Query of Prescription Drug Monitoring Program (PDMP) (5 bonus points)
- Verify Opioid Treatment Agreement) (5 bonus points)
- Health Information Exchange:
- Support Electronic Referral Loops By Sending Health Information Measure (20 points)
- Support Electronic Referral Loops By Receiving and Incorporating Health Information (20 points)
- Provider to Patient Exchange:
- Provide Patients Electronic Access to Their Health Information (40 points)
- Public Health and Clinical Data Exchange (choose 2 for a total of 10 points)
- Immunization Registry Reporting,
- Electronic Case Reporting,
- Public Health Registry Reporting,
- Clinical Data Registry Reporting,
- Syndromic Surveillance Reporting)
- Removed measures
- Request/Accept Summary of Care
- Clinical Information Reconciliation
- Patient-Specific Education
- Secure Messaging
- View, Download or Transmit
- Patient-Generated Health Data
- e-Prescribing:
- Continues exclusions for the EPrescribing and Health Information Exchange Measures.
- For small practices (15 or fewer clinicians), adds a new category of hardship exceptions to re-weight Advancing Care Information performance category to 0 and reallocate the Advancing Care Information performance category weight of 25% to the Quality performance category.
- CMS will reweight the Promoting Interoperability performance category to 0 and reallocate the performance category weight of 25% to the Quality performance category for the following reasons:
- Automatic reweighting:
- Hospital-based MIPS eligible clinicians;
- Non-Patient Facing clinicians;
- Ambulatory Surgical Center (ASC)— based MIPS eligible clinicians, finalized retroactive to the transition year;
- Nurse practitioners, physician assistants, clinical nurse specialist, certified registered nurse anesthetists;
- Reweighting extends to additional clinician types (physical therapists, occupational therapists, speech-language pathologists, audiologists, clinical psychologists and registered dietitians and nutrition professionals).
- Reweighting through an approved application:
- New hardship exception for clinicians in small practices (15 or fewer clinicians);
- New decertification exception for eligible clinicians whose EHR was decertified, retroactively effective to performance periods in 2017.
- Significant hardship exceptions—CMS will not apply a 5-year limit to these exceptions;
- Automatic reweighting:
- Cost:
- Weight to final score: 15% (instead of 10% in 2018)
- CMS is including the Medicare Spending per Beneficiary (MSPB) and total per capita cost measures to calculate your Cost performance category score for the 2019 MIPS performance period.
- Case minimum of 35 for the MSPB measure and 20 for the total per capita cost measure.
- Episode-Based Measures will be added to the list of Cost measures for the 2019 MIPS Performance Period and Future Performance Periods:
- Elective Outpatient Percutaneous Coronary Intervention (PCI) (Procedural)
- Knee Arthroplasty (Procedural)
- Revascularization for Lower Extremity Chronic Critical Limb Ischemia (Procedural)
- Routine Cataract Removal with Intraocular Lens (IOL) Implantation (Procedural)
- Screening/Surveillance Colonoscopy (Procedural)
- Intracranial Hemorrhage or Cerebral Infarction (Acute inpatient medical condition)
- Simple Pneumonia with Hospitalization (Acute inpatient medical condition)
- ST-Elevation Myocardial Infarction (STEMI) with Percutaneous Coronary Intervention (PCI) (Acute inpatient medical condition)
- Case minimum of 10 for procedural episodes and 20 for acute inpatient medical condition episodes
- CMS will calculate cost measure performance; no action is required from clinicians.
Additional Details:
- CMS estimate that between 165,000 and 220,000 clinicians will become Qualifying APM Participants (QP). As a QP, an eligible clinician is exempt from the MIPS reporting requirements and payment adjustment, and qualifies for a lump sum incentive payment based on 5 percent of their aggregate payment amounts for covered professional services for the prior year. CMS estimates that the total lump sum APM incentive payments will be approximately $600-800 million for the 2021 Quality Payment Program payment year.
- Offering the Virtual Groups participation option. The 2019 rule offers again Virtual Group participation, which is another way clinicians can elect to participate in MIPS.
- For 2019, a designated virtual group representative must e-mail a virtual group election to MIPS_VirtualGroups@cms.hhs.gov by December 31 of the calendar year prior to the start of the applicable performance period
- Non-Patient Facing: There is no change in how CMS is defining non-patient facing clinicians (Individual’s ≤100 patient facing encounters. Groups: > 75% NPIs billing under the group’s TIN during a performance period are labeled as non-patient facing.) however; CMS is using the same definition for Virtual Groups. Virtual Groups: > 75% NPIs within a Virtual Group during a performance period are labeled as non-patient facing.
- Providing the option to use facility-based scoring for facility-based clinicians that doesn’t require data submission.
- Complex Patients Bonus: Apply an adjustment of up to 5 bonus points by adding the average Hierarchical Conditions Category (HCC) risk score to the final score. Generally, this will award between 1 to 5 points to clinicians based on the medical complexity of the patients they see.
- Small Practice Bonus:
- The small practice bonus is increased to 6 points and will now be added to the Quality performance category, rather than in the MIPS final score calculation.
- Extreme and Uncontrollable Circumstances Payment adjustments:
- CMS will automatically reweight the Quality, Improvement Activities, Cost and Promoting Interoperability performance categories for MIPS eligible clinicians who are affected by extreme and uncontrollable circumstances affecting entire regions or locales.