Twenty (20) cost measures, including 10 new Episode-based measures, are used to evaluate performance in the Cost performance category in the 2020 MIPS performance period. CMS uses Medicare claims data to calculate cost measure performance which means clinicians do not have to submit any data for this performance category.
- Medicare Spending Per Beneficiary (MSPB) Clinician - New for 2020: Refined attribution methodology for medical and surgical episodes; Service exclusions for costs that are unlikely to be influenced by clinicians
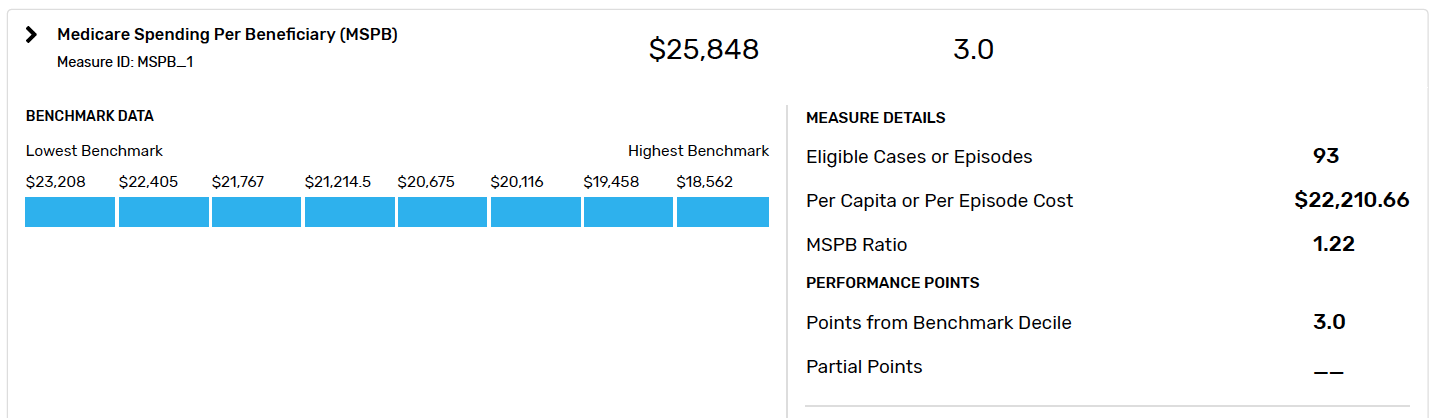
The Medicare Spending Per Beneficiary (MSPB) measure evaluates solo practitioners and groups on their spending efficiency and is risk-adjusted to account for patients' risk profiles. Solo practitioners and groups are identified by their National Provider Identification (NPI) and Taxpayer Identification Number (TIN) combination. Specifically, the MSPB measure assesses the average spend for Medicare services performed by providers/groups per episode of care. Each episode comprises the period immediately prior to, during, and following a patient's hospital stay. Each beneficiary MSPB episode is attributed to a single TIN-NPI.
The episode is attributed to the MIPS eligible clinician who billed the plurality of Medicare Part B claims, measured by allowed charges, during the period between the index admission date and the discharge date.
- Total Per Capita Costs (TPCC) - New for 2020: Refined attribution methodology for identifying primary care relationships; Specialty exclusions for clinicians who don’t provide primary care services; Refined risk adjustment to account for changes in patient health status during the year
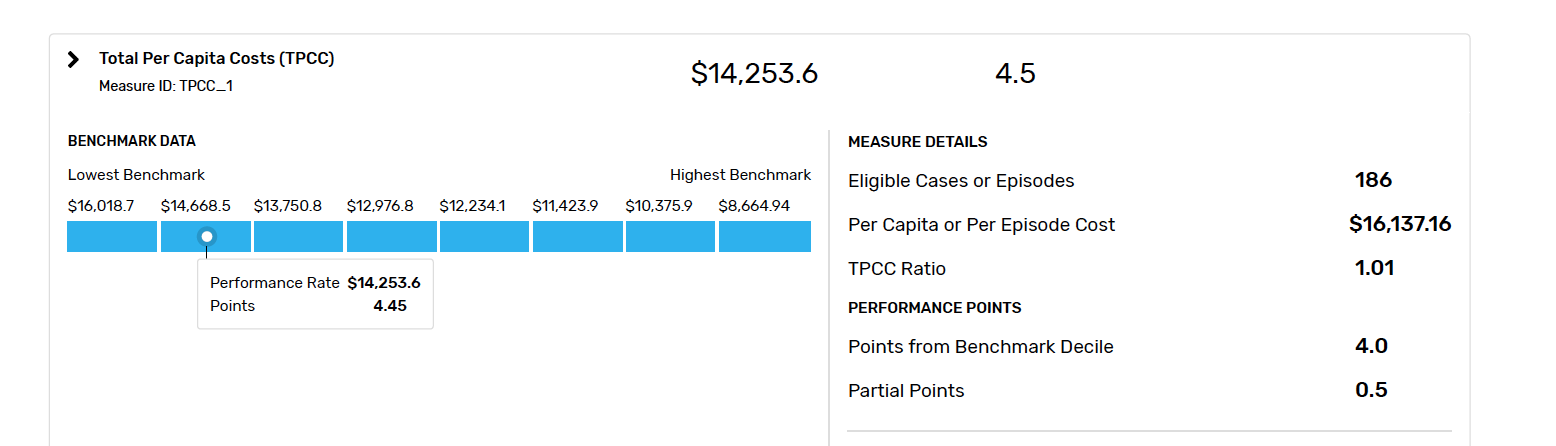
The Total Per Capita Costs (TPCC) measure is a payment-standardized, annualized, risk-adjusted, and specialty-adjusted measure that evaluates the overall efficiency of care provided to beneficiaries attributed to solo practitioners and groups, as identified by their Medicare Taxpayer Identification Number (TIN). On the attribution logic to TPCC there are 2 steps:
Step 1: If a beneficiary received more primary care services from an individual TIN-NPI that is classified as either a primary care physician (PCP), nurse practitioner (NP), physician assistant (PA) or clinical nurse specialist (CNS) than from any other TIN-NPI during the performance period, then the beneficiary is attributed to that TIN-NPI.
Step 2: If a beneficiary did not receive a primary care service from a TIN-NPI classified as either a PCP, NP, PA or CNS during the performance period, then the beneficiary may be assigned to a TIN-NPI in "Step 2."
- 18 Episode-Based Measures (10 added for PY2020)
These measures assess the cost of care (Medicare Parts A and B claims) that are related to a specific episode of care for a clinical condition or procedure. The measures are categorized into "episode groups" (e.g., procedural episodes or acute inpatient medical condition episodes).
Benchmarks
CMS will establish a single, national benchmark for each cost measure. These benchmarks are based on the performance period, not a historical baseline period. As a result, CMS can’t publish the actual numerical benchmarks for the cost measures before the start of each performance period. For example, the MSPB benchmark used to determine a MIPS eligible clinician’s 2020 Cost performance category score will be based on CY 2020 claims data. All MIPS eligible clinicians that meet or exceed the case minimum for a measure are included in the same benchmark. Case minimums for each cost measure are identified below.
- MSPB - A clinician must have a minimum of 35 eligible cases.
- TPCC - A clinician must have a minimum of 20 eligible cases.
- Episode-based measures - The minimum case volume for procedural episode-based measures is 10. The minimum case volume for acute inpatient medical condition episode-based measures is 20.
When Will Facility-Based Measures Scoring Apply?
Facility-based measurement scoring will be used for your Quality and Cost performance category scores when:
- You are identified as facility-based on your QPP participation page;
- You are attributed to a facility with a FY 2021 Hospital Value Based Purchasing (VBP) Program score; and
- The Hospital VBP Program score results in a higher combined Quality and Cost score than the MIPS Quality measure data you submit and MIPS Cost measure data CMS calculates for you.