The MIPS Improvement Activities (IA) performance category measures participation in activities that improve clinical practice. This category is 15% (or up to 15 points) of your MIPS score. Small practices that do not report the Promoting Interoperability category of MIPS will have the IA category re-weighted to 30% (or up to 30 points of their score).
*NEW IN 2025: Improvement activities will no longer be weighted, and the number of activities clinicians are required to attest to completing has changed:
- MVP Reporting: Clinicians, groups, and subgroups (regardless of special status) must attest to 1 activity
- Traditional MIPS Reporting:
- Clinicians, groups, and virtual groups with the small practice, rural, non-patient facing, or health professional shortage area special status must attest to 1 activity.
- All other clinicians, groups, and virtual groups must attest to 2 activities.
All Improvement Activities can be easily attested to with MDinteractive.
- Log into your account
- Click on Add/Edit next to the IA category. This will direct you to the IA reporting module. Note that you might have to enter your NPI/TIN combination or just TIN (if reporting as a group) to be able to see the categories and Add/Edit.
- Enter your minimum 90 day reporting period at the top.
- Click “Add” to each activity that you performed for at least 90 consecutive days in 2025. Only add activities after reviewing the instructions to confirm you can provide supporting documentation if audited. Attesting to more than the required number of activities will not increase your score.
- Upload supporting documentation for the activities you have attested to.
Note: There are frequency restrictions associated with the following Improvement Activities: IA_PSPA_4, IA_PSPA_22, and IA_PSPA_23. Please review the documentation/rules for these activities prior to attestation.
To achieve the maximum 15 points* for the Improvement Activities score:
- Clinicians, groups, virtual groups, and APM Entities with certain special statuses (small practice with 15 or fewer providers; rural, health professional shortage area (HPSA); non-patient facing) must attest to 1 activity.
- All other clinicians must attest to 2 activities.
Important: Group reporting (reporting on the TIN level) requires that at least 50% of those in the TIN have completed the activity/activities being attested to.
*Up to 30 points for individuals or small practices that do not report Promoting Interoperability.
Tips: Improvement Activities are sorted into the following subcategories which might assist you with locating activities that apply to your practice:
- Achieving Health Equity (AHE): Engagement of new Medicaid patients and follow-up.
- Behavioral and Mental Health (BMH): Activities that look at the co-morbidity of mental health and physical health. Some cross-over with Quality measures.
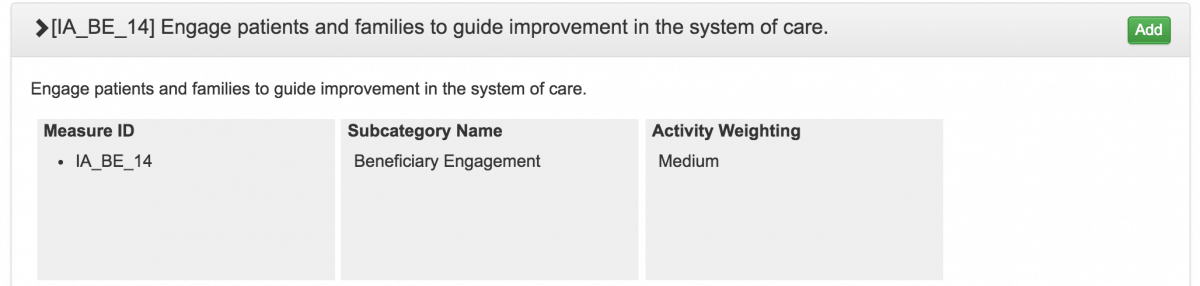
- Beneficiary Engagement (BE): Engagement of patients through post-visit surveys, tracking reported outcomes, using care plans to manage chronic conditions.
- Care Coordination (CC): Coordination of care between clinicians. health information exchange, coordinated planning, etc.
- Emergency Response & Preparedness (ERP): Supporting communities by registering to be part of a disaster relief team or participation in supporting humanitarian needs.
- Expanded Practice Access (EPA): How accessible are you to your beneficiaries?
- Patient Safety and Practice Assessment Population Management (PSPA): Patient safety monitoring programs (i.e., prescription drug monitoring, appropriate use of antibiotics, etc.)
- Population Management (PM): Population health. Using research, tools, etc.
- Note: The MDinteractive Suggestions by Specialty pages include recommendations for activities a clinician or group might be able to attest to.
Here are suggestions regarding the documentation you should have for any attested to Improvement Activity:
- List the start date and end date for each activity
- Describe the goals, outcomes, or metrics for each activity
- Describe the process being improved and the benefit of improving the process
- List the staff involved for each activity
- List the technology used. If possible take screenshots
- Describe workflows
- Document improvement activities compliance
- Describe monitoring systems to gauge your progress towards the goals
- Store all documentation in computer files