
On November 2, 2021, the Centers for Medicare and Medicaid Services (CMS) issued the Final Rule for the 2022 Medicare Physician Fee Schedule (PFS) which includes several changes to the Quality Payment Program (QPP). The Rule makes significant revisions to the existing MIPS program and outlines a timeframe for transitioning to the new MIPS Value Pathways (MVPs). Here are the key takeaways that will have a major impact on the future of clinician reporting.
Changes to Traditional MIPS
The Quality Payment Program (QPP) was originally established in 2017 with two payment tracks that clinicians could choose from which included MIPS and Advanced Alternative Payment Models (APMs). “Traditional MIPS” refers to this original framework available to MIPS eligible clinicians for collecting and reporting data.
CMS has adopted substantial policy changes to traditional MIPS reporting in 2022 and future years.
MIPS Eligible Clinicians
Two new clinician types are added to the existing list of MIPS eligible clinicians beginning with the 2022 performance year:
- Clinical social workers
- Certified nurse-midwives
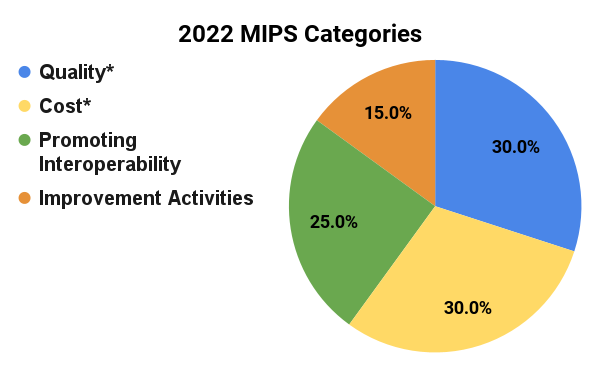
MIPS Performance Category Weight Changes
By law, the Quality and Cost performance categories must be equally weighted at 30% beginning with the 2022 performance period. The weights for the Promoting Interoperability (25%) and Improvement Activities (15%) categories will remain the same as 2021.
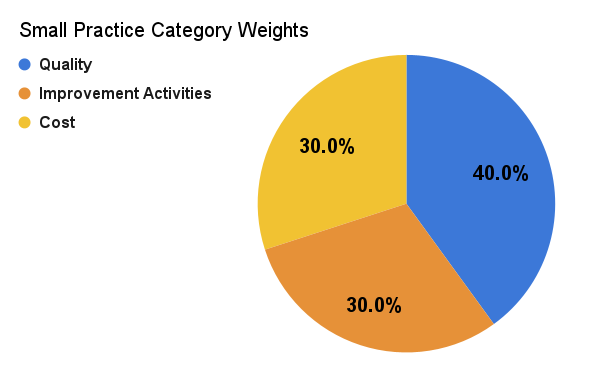
Redistributing Performance Category Weights for Small Practices
The Final Rule updates the performance category weights for small practice clinicians. Small practice clinicians will have PI automatically reweighted (no application required). The other categories will be reweighted as follows:
If the small practice reports PI data, the category will be scored and the normal weights will apply.
In cases where both the Cost and the PI categories are reweighted the Quality and Improvement Activities categories will be equally weighted at 50%.
Minimum Performance Threshold and Payment Adjustments
CMS is required to establish a performance threshold that is either the mean or medium of the final MIPS scores for all MIPS eligible clinicians for a prior performance period beginning with the 2022 performance year. The agency has finalized a minimum performance threshold of 75 MIPS points in 2022 (up from 60 MIPS points in 2021) which is the mean final score from the 2017 performance year. Next year clinicians will need to achieve a final MIPS score of at least 75 points to avoid any MIPS penalty.
An additional performance threshold of 89 points is established for exceptional performance. The 2022 performance year is the last year for an additional MIPS adjustment for exceptional performance.
The maximum payment adjustments for 2022 remain the same at +/- 9% and will be applied towards a clinician’s 2024 Medicare Part B payments for covered professional services. This means a MIPS eligible clinician who does not participate in MIPS in 2022 will receive a negative payment adjustment of -9% in 2024.
2022 Reweighting Policies
Large Practice Participants
The table below illustrates the 2022 performance category reweighting policies that CMS will apply to large practice participants (practice has 16 or more clinicians):
Reweighting Scenario | Quality | Cost | Improvement Activities (IA) | Promoting Interoperability (PI) |
|---|---|---|---|---|
| No Reweighting Needed | ||||
| Scores for all 4 performance categories | 30% | 30% | 15% | 25% |
| Reweight 1 Performance Category | ||||
| No Cost | 55% | 0% | 15% | 30% |
| No PI | 55% | 30% | 15% | 0% |
| No Quality | 0% | 30% | 15% | 55% |
| No IA | 45% | 30% | 0% | 25% |
| Reweight 2 Performance Categories | ||||
| No Cost and no PI | 85% | 0% | 15% | 0% |
| No Cost and no Quality | 0% | 0% | 15% | 85% |
| No Cost and no IA | 70% | 0% | 0% | 30% |
| No PI and no Quality | 0% | 50% | 50% | 0% |
| No PI and no IA | 70% | 30% | 0% | 0% |
| No Quality and no IA | 0% | 30% | 0% | 70% |
Small Practice Participants
The table below illustrates the 2022 performance category reweighting policies that CMS will apply to small practice participants (practice has 15 or fewer clinicians):
| Reweighting Scenario | Quality | Cost | Improvement Activities (IA) | Promoting Interoperability (PI) |
|---|---|---|---|---|
| No Reweighting Needed | ||||
| Scores for all 4 performance categories | 30% | 30% | 15% | 25% |
| Reweight 1 Performance Category | ||||
| No Cost | 55% | 0% | 15% | 30% |
| No PI* | 40% | 30% | 30% | 0% |
| No Quality | 0% | 30% | 15% | 55% |
| No IA | 45% | 30% | 0% | 25% |
| Reweight 2 Performance Categories | ||||
| No Cost and no PI* | 50% | 0% | 50% | 0% |
| No Cost and no Quality | 0% | 0% | 15% | 85% |
| No Cost and no IA | 70% | 0% | 0% | 30% |
| No PI and no Quality | 0% | 50% | 50% | 0% |
| No PI and no IA | 70% | 30% | 0% | 0% |
| No Quality and no IA | 0% | 30% | 0% | 70% |
*The finalized redistribution policy specifically for MIPS eligible clinicians in small practices.
Quality Category
CMS finalized several changes to the MIPS Quality category.
- Data Completeness - MIPS eligible clinicians will continue to meet the current data completeness threshold of 70% (e.g., must report at least 70% of eligible cases for each Quality measure) for the 2022 and 2023 performance periods.
- Quality Measure Scoring - Scoring updates will be applied to new measures and measures that do not meet case minimum and data completeness requirements, and measures that do not have a benchmark.
- New Quality measures - In 2022 a 7-point floor is established for the first performance period and a 5-point floor for the second performance period for new Quality measures.
- Beginning with the 2023 performance period:
- Measures with a benchmark - The 3-point floor is removed for measures that can be scored against a benchmark. These measures will receive 1-10 points.
- Measures without a benchmark - The 3-point floor is removed for measures without a benchmark (except small practices). These measures will receive 0 points (small practices will continue to earn 3 points).
- Measures that don’t meet case minimum requirements (20 cases) - The 3-point floor is removed (except small practices). These measures will earn 0 points (small practices will continue to earn 3 points).
- Bonus Points - Bonus points will no longer be awarded in 2022 for end-to-end (ETE) electronic reporting and reporting additional Outcome/High-priority measures beyond the required measures.
- Scoring for Groups Reporting Claims Measures - CMS will only calculate a group-level Quality category score from Medicare Part B Claims measures if the practice submitted data for another performance category as a group (signaling their intent to participate as a group).
- CMS Web Interface - The CMS Web Interface will be extended as a collection type and submission type in traditional MIPS for registered groups, virtual groups, and APM Entities with 25 or more clinicians for the 2022 performance period. It will continue to be a reporting option for Medicare Shared Savings Program ACOs through 2024.
- Quality Measures - There are 200 Quality measures available for the 2022 performance period. This includes substantive changes to 87 existing Quality measures, one new specialty measure set for certified nurse-midwives, four new Quality measures (including 1 new administrative claims measure), and removal of 15 existing Quality measures (two are applicable to Medicare Part B Claims only).
| Measures to be Removed | New Quality Measures | New Administrative Claims Measure |
|---|---|---|
#14 Age-Related Macular Degeneration (AMD): Dilated Macular Examination for Medicare Part B Claims type only | #481 - Intravesical Bacillus-Calmette Guerin for Non-muscle Invasive Bladder Cancer | Clinician and Clinician Group Risk-standardized Hospital Admission Rates for Patients with Multiple Chronic Conditions |
| #21 Perioperative Care: Selection of Prophylactic Antibiotic – First OR Second-Generation Cephalosporin | #482 - Hemodialysis Vascular Access: Practitioner Level Long-term Catheter Rate | |
| #23 Perioperative Care: Venous Thromboembolism (VTE) Prophylaxis (When Indicated in ALL Patients) | #483 - Person-Centered Primary Care Measure Patient-Reported Outcome Performance Measure (PCPCM PRO-PM) | |
| #44 Coronary Artery Bypass Graft (CABG): Preoperative Beta-Blocker in Patients with Isolated CABG Surgery | ||
| #50 Urinary Incontinence: Plan of Care for Urinary Incontinence in Women Aged 65 Years and Older for Medicare Part B Claims type only | ||
| #67 Hematology: Myelodysplastic Syndrome (MDS) and Acute Leukemias: Baseline Cytogenetic Testing Performed on Bone Marrow | ||
| #70 Hematology: Chronic Lymphocytic Leukemia (CLL): Baseline Flow Cytometry | ||
| #154 Falls: Risk Assessment | ||
| #195 Radiology: Stenosis Measurement in Carotid Imaging Reports | ||
| #225 Radiology: Reminder System for Screening Mammograms | ||
| #337 Psoriasis: Tuberculosis (TB) Prevention for Patients with Psoriasis, Psoriatic Arthritis and Rheumatoid Arthritis on a Biological Immune Response Modifier | ||
| #342 Pain Brought Under Control Within 48 Hours | ||
| #429 Pelvic Organ Prolapse: Preoperative Screening for Uterine Malignancy | ||
| #434 Proportion of Patients Sustaining a Ureter Injury at the Time of Pelvic Organ Prolapse Repair | ||
| #444 Medication Management for People with Asthma |
Cost Category
The Final Rule will add five newly developed episode-based Cost measures for the 2022 performance period.
- 2 procedural measures: Melanoma Resection, Colon and Rectal Resection
- 1 acute inpatient measure: Sepsis
- 2 chronic condition measures: Diabetes, Asthma/Chronic Obstructive Pulmonary Disease [COPD]
Improvement Activities (IA) Category
CMS will update the Improvement Activities inventory for the 2022 performance year, including adding seven new activities and modifying 15 current activities. Many of the changes pertain to health equity and standardizing language related to equity across the activities. There are six activities that will be removed from the IA inventory.
The Final Rule will also allow CMS to suspend an Improvement Activity if there is a reason to believe that the continued collection raises possible patient safety concerns or is obsolete. In these cases, CMS would immediately notify clinicians and the public through the usual communication channels and would then propose to remove or modify the activity as appropriate in the next rulemaking cycle.
| Improvement Activities to be Removed | New Improvement Activities |
|---|---|
| IA_ BE_13 Regularly assess the patient experience of care through surveys, advisory councils and/or other mechanisms | IA_AHE_8 - Create and Implement an Anti-Racism Plan (High) |
| IA_PSPA_11 - Participation in CAHPS or other supplemental questionnaire | IA_AHE_9 Implement Food Insecurity and Nutrition Risk Identification and Treatment Protocols (Medium) |
| IA_BE_17 - Use of tools to assist patient self-management | IA_BMH_11 - Implementation of a Trauma-Informed Care (TIC) Approach to Clinical Practice (Medium) |
| IA_BE_18 - Provide peer-led support for self-management. | IA_BMH_12 - Promoting Clinician Well-Being (High) |
| IA_BE_20 - Implementation of condition-specific chronic disease self-management support programs | IA_ERP_4 - Implementation of a Personal Protective Equipment (PPE) Plan (Medium) |
| IA_BE_21 - Improved practices that disseminate appropriate self-management materials | IA_ERP_5 - Implementation of a Laboratory Preparedness Plan (Medium) |
| IA_PSPA_33 - Application of CDC’s Training for Healthcare Providers on Lyme Disease (Medium) |
Promoting Interoperability (PI) Category
CMS will apply automatic reweighting to the following, beginning with the 2022 performance period:
- Clinical social workers
- Small practices
Note there is no automatic reweighting for certified nurse-midwives.
The following changes have also been adopted to the PI reporting requirements:
- Revises reporting requirements for the Public Health and Clinical Data Exchange objective to support public health agencies (PHAs) in future health threats and a long term COVID-19 recovery.
- CMS will require reporting of the Immunization Registry Reporting and Electronic Case Reporting (unless an exclusion can be claimed).
- The Public Health Registry Reporting, Clinical Data Registry Reporting, and Syndromic Surveillance Reporting measures will be optional and MIPS eligible clinicians could earn 5 bonus points if they report a “yes” response for any one of them. Note reporting more than one of these optional measures won’t result in more than 5 bonus points.
- Adopts a new required measure called the Safety Assurance Factors for EHR Resilience Guides (SAFER Guides). This measure requires MIPS eligible clinicians to attest to conducting an annual assessment of the SAFER Guides beginning with the 2022 performance period.
- Adds a fourth exclusion to the Electronic Case Reporting for the 2022 performance period only: Uses certified electronic health record technology (CEHRT) that isn’t certified to the electronic case reporting certification criterion prior to the start of the performance period they select in 2022.
- Modifies the Prevention of Information Blocking attestation statements.
Complex Patient Bonus
CMS will continue doubling the complex patient bonus for the 2021 MIPS performance year. These bonus points (capped at 10-points) will be added to the final score. The agency is also revising the complex patient bonus beginning with the 2022 MIPS performance year by:
- Limiting the bonus to clinicians who have a median or higher value for at least one of the two risk indicators (Hierarchical Condition Category (HCC) and proportion of patients dually eligible for Medicare and Medicaid benefits).
- Updating the formula to standardize the distribution of two risk indicators so that the policy can target clinicians who have a higher share of socially and/or medically complex patients.
- Increasing the bonus to a maximum of 10.0 points.
Facility-based measurement
Some clinicians and practices are designated as facility-based and eligible for special scoring. CMS is adopting the following changes to facility-based measurement for the 2022 performance year:
- The MIPS Quality and Cost performance category scores will be based on the facility-based measurement scoring methodology unless a clinician or group receives a higher MIPS final score through another MIPS submission.
2022 MIPS Reporting Webinars
Clinicians can view our 2022 MIPS reporting webinars for step-by-step instructions on how to get started with their 2022 MIPS reporting:
- 2022 MIPS Reporting for Small Practices (15 or fewer clinicians)
- 2022 MIPS Reporting for Large Practices (16 or more clinicians)
The Future of the Quality Payment Program
While MIPS has gone through incremental changes since its inception in 2017, CMS intends to transform the program in future years through the adoption of the MIPS Value Pathways (MVPs) and the APM Performance Pathway (APP).
MVPs
Clinicians will be able to report MVPs beginning with the 2023 performance year as a new reporting framework to eventually replace the traditional MIPS program. MVPs will be voluntary for the 2023 to 2027 performance years.
The purpose of MVPs is to align and connect measures and activities across the MIPS Quality, Cost, Promoting Interoperability, and Improvement Activities performance categories for different specialties or conditions. CMS finalized seven MVPs for the 2023 performance year:
- Advancing Rheumatology Patient Care
- Coordinating Stroke Care to Promote Prevention and Cultivate Positive Outcomes
- Advancing Care for Heart Disease
- Optimizing Chronic Disease Management
- Adopting Best Practices and Promoting Patient Safety within Emergency Medicine
- Improving Care for Lower Extremity Joint Repair
- Support of Positive Experiences with Anesthesia
More information about MVP reporting and the future of the MIPS program can be found here.
APP
In the 2021 Final Rule for the QPP, CMS introduced a new reporting framework for MIPS Alternative Payment Models (APMs) and Accountable Care Organizations (ACOs) called the APM Performance Pathway (APP). The APP is a single, pre-determined measure set that MIPS APM participants may choose to report on beginning in the 2021 performance year.
Medicare Shared Savings Program (MSSP) ACOs can continue reporting Quality data through the CMS Web Interface through the 2024 performance year. However, in 2025 they will have to report all-payer Quality data on three eCQMs/MIPS CQMs via the APP.
More information about the APP can be found here.
FHIR and Digital Quality Measures (dQMs)
CMS aims to move fully to digital quality measures (dQMs) for quality reporting using Fast Healthcare Interoperability Resources (FHIR) by 2025. FHIR is a free and open-source standards framework (in both commercial and government settings) created by Health Level Seven International (HL7®) that establishes a common language and process for all health IT. It allows systems to communicate and information to be shared seamlessly with a lower burden on stakeholders.
CMS plans to align eCQMs with the FHIR standard and support quality measurement via application programming interfaces (APIs). One key goal of the plan is to improve the efficiency of quality reporting by moving to digital measures and using advanced data analytics. CMS believes FHIR standards enable collaboration and information sharing, which is essential for delivering high-quality care and better outcomes at a lower cost. By aligning technology requirements for payers, health care providers, and health IT developers CMS can advance an interoperable health IT infrastructure that ensures providers and patients have access to health data when and where it is needed.
The ONC 21st Century Cures Act created a Standardized API for Patient and Population Services certification criterion for health IT that requires the use of FHIR Release 4 and several implementation specifications. Health IT certified to this criterion will offer single patient and multiple patient services that can be accessed by third-party applications like MDinteractive registry. The rule also requires health IT developers to update their certified health IT to support the United States Core Data for Interoperability (USCDI) standard by December 31, 2022.
The use of APIs will reduce longstanding barriers to quality measurement. Currently, integrating between different health IT systems is burdensome and costly, and it is difficult to reliably obtain high quality data across EHRs. As health IT developers map their health IT data to the FHIR standard, APIs can enable structured data to be easily accessible for quality measurement or other use cases, such as care coordination, clinical decision support, and supporting patient access.
The Rule describes 4 future actions that would enable the transformation to a fully digital quality measurement enterprise by 2025:
- Leveraging and Advancing Standards for Digital Data and Obtaining all EHR Data Required for Quality Measures via Provider FHIR-based APIs.
- Redesigning Quality Measures to be Self-Contained Tools.
- Building a Pathway to Data Aggregation in Support of Quality Measurement.
- Potential Future Alignment of Measures Across Reporting Programs, Federal and State Agencies, and the Private Sector
Next Steps
The 2022 Final Rule makes significant changes to the traditional MIPS program next year and lays out a plan to introduce MVP reporting. MIPS eligible clinicians should begin reviewing these changes now so they understand the potential impact on their reporting practices.
Leave a comment