
As CMS transitions ACOs to all-payer, all-patient CQM/eCQM reporting under the APP, the complexity of quality reporting is increasing. MDinteractive supports over two dozen ACOs—ranging from 37 to over 7,000 clinicians—with scalable tools and expert guidance. Our platform simplifies data aggregation across EHRs, ensures compliance, and provides real-time performance insights to help ACOs meet evolving regulatory requirements with confidence.
As Alternative Payment Models (APMs) continue to reshape the healthcare landscape, Accountable Care Organizations (ACOs) are under increasing pressure to meet quality reporting requirements efficiently and accurately. The latest updates from CMS regarding CQM (Clinical Quality Measures) and eCQM (electronic Clinical Quality Measures) reporting represent both a challenge and an opportunity for ACOs navigating the evolving regulatory environment. At MDinteractive, we’ve made it our mission to empower ACOs with the tools, experience, and support they need to succeed.
Understanding the Shift: CQM/eCQM Requirements for ACOs
Under the Medicare Shared Savings Program (MSSP), ACOs are now required to report quality data through the Alternative Payment Model Performance Pathway (APP). The APP includes four quality measures that must be submitted via CQMs or eCQMs.
ACOs must report at least 75% of their eligible population. This change significantly increases the scope and complexity of quality data collection and submission, requiring a comprehensive and coordinated approach across the ACO’s Taxpayer Identification Numbers (TINs) and National Provider Identifiers (NPIs).
MDinteractive’s Deep Bench of ACO Experience
MDinteractive is proud to be a trusted reporting partner for over two dozen ACOs across the country. These ACOs represent a diverse spectrum, with:
-
A range of 1 to 110 TINs per ACO, with a median of 50 TINs
-
Ranging from 37 clinicians to more than 7,080 clinicians
-
A median clinician count of 1,320 per ACO
This scale and diversity demonstrate our ability to support a wide range of ACO configurations—from smaller, regionally focused networks to large, national organizations.
Our platform is purpose-built to handle the intricacies of ACO-level data aggregation and normalization, supporting both CQM and eCQM submissions with ease. Whether your organization is preparing for its first APP reporting year or optimizing an ongoing quality strategy, MDinteractive brings unparalleled scalability and adaptability.
ACO Submission Types Trends
Among the ACOs we support, there’s a diverse range of quality reporting strategies. Based on recent data, here’s how submission types were distributed:
-
Medicare CQM – 55%
-
eCQM – 15%
-
MIPS CQM – 15%
-
MIPS CQM and Medicare CQM – 5%
-
eCQM and Medicare CQM – 5%
-
eCQM and MIPS CQM – 5%
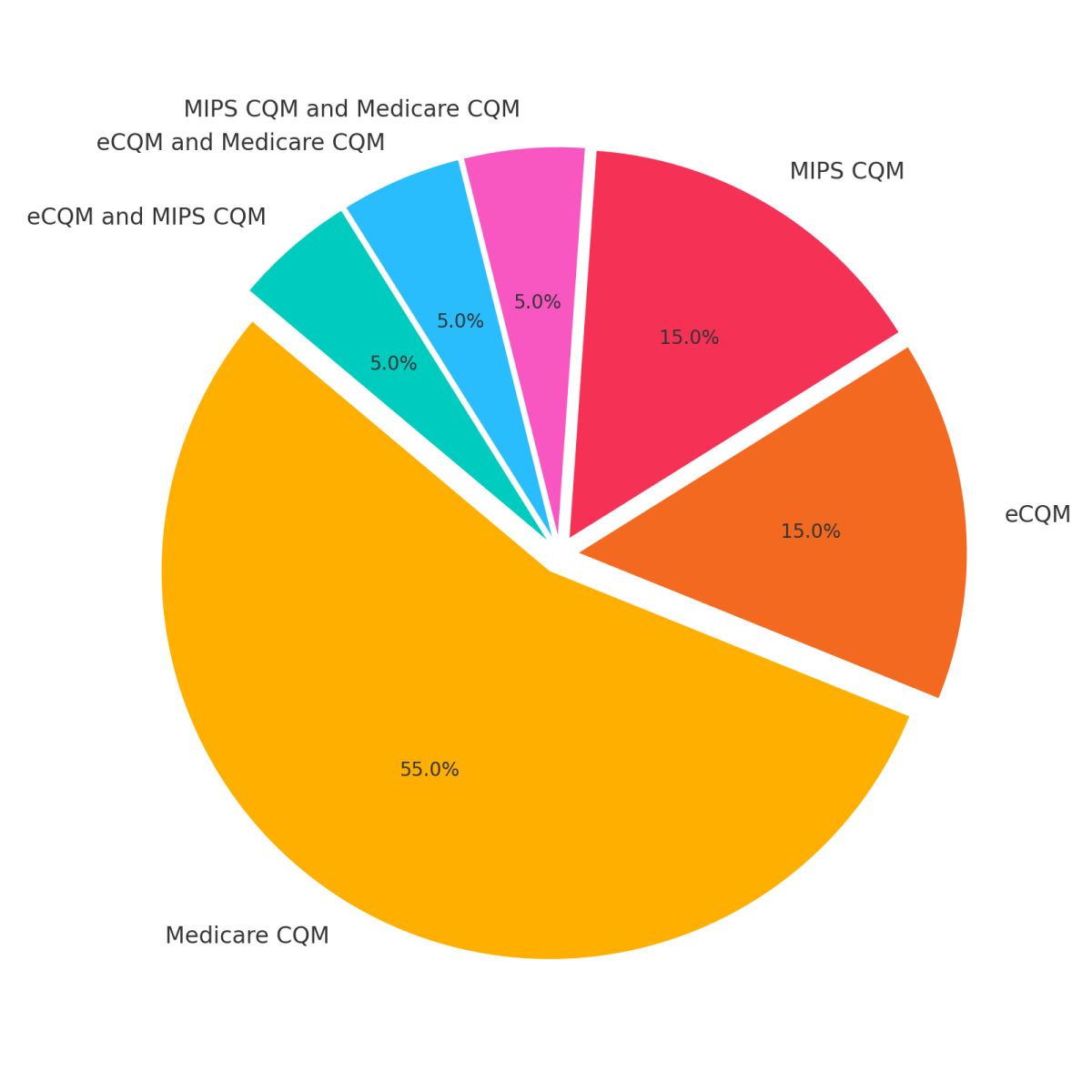
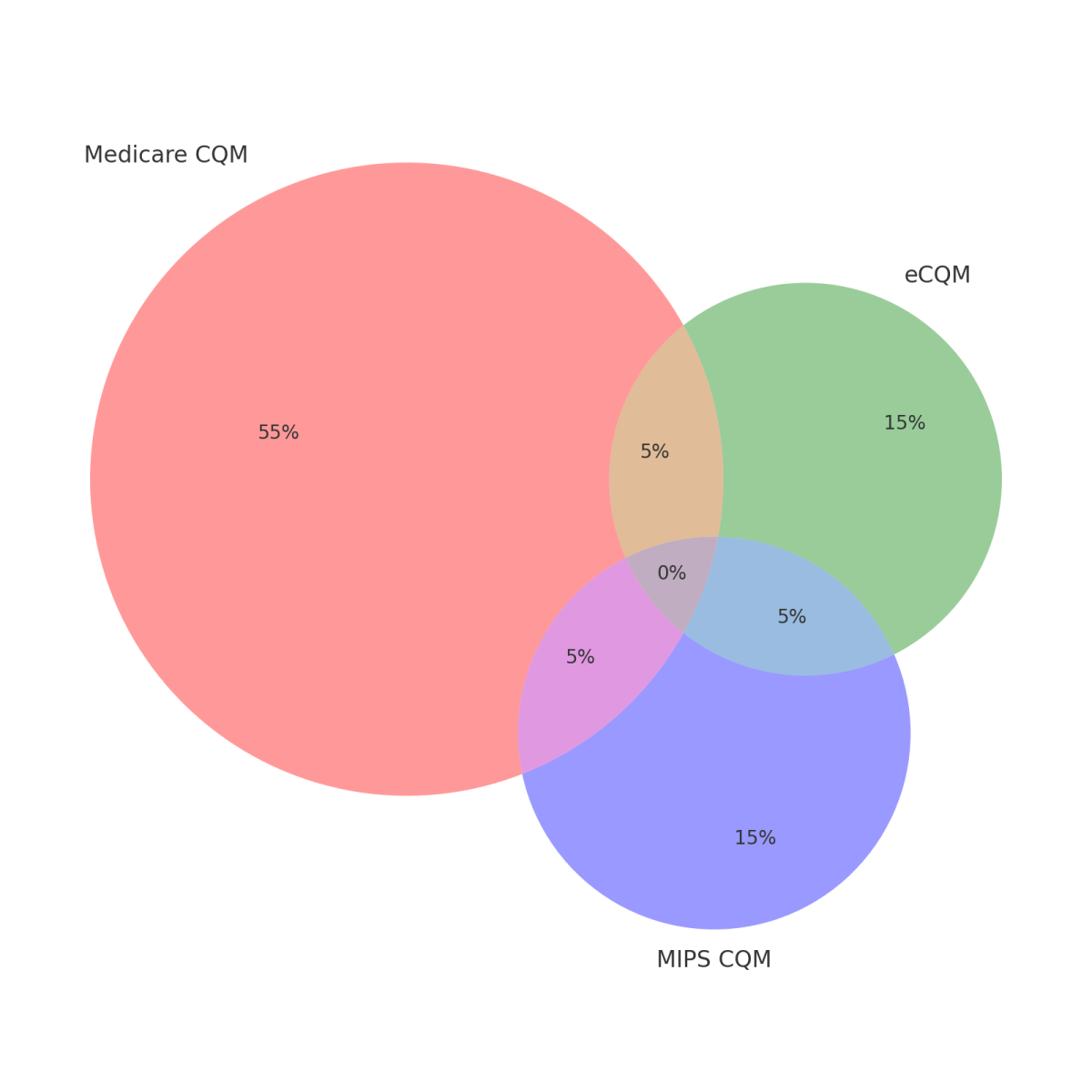
These numbers highlight a strong trend toward Medicare CQM submissions, but also reveal increasing interest in hybrid strategies that combine MIPS CQMs and eCQMs to align with varied data environments and EHR capabilities.
ACO Performance Summary by Measure and Collection Type
| ACO Performance Summary by Measure and Collection Type | ||||
|---|---|---|---|---|
| Measure ID | Collection Type | Mean Perf. | Min Perf. | Max. Perf. |
| 001 | CQMs | 36% | 29% | 50% |
| 001 | eCQMs | 39% | 19% | 69% |
| 001SSP | CQMs | 32% | 18% | 57% |
| 134 | CQMs | 37% | 4% | 55% |
| 134 | eCQMs | 21% | 0% | 34% |
| 134SSP | CQMs | 45% | 25% | 64% |
| 236 | CQMs | 69% | 64% | 71% |
| 236 | eCQMs | 77% | 72% | 86% |
| 236SSP | CQMs | 73% | 65% | 81% |
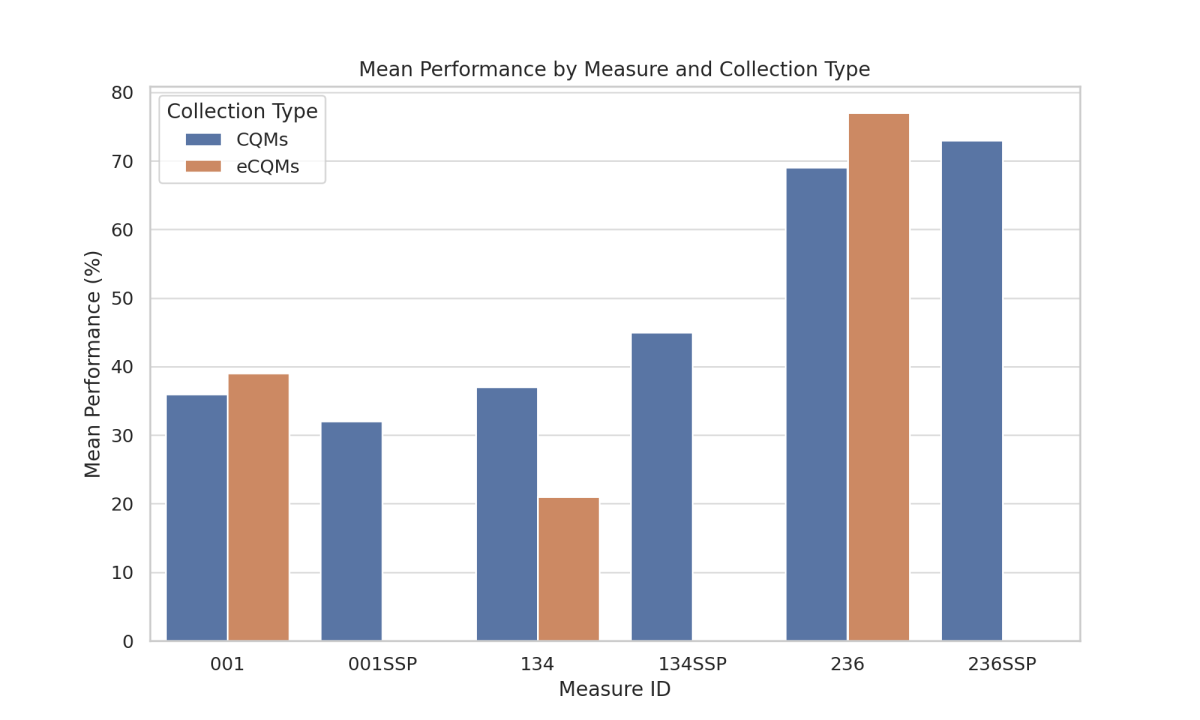
Measure Legend
-
The "SSP" suffix (e.g., 001SSP) indicates that the measure is part of the Medicare CQMs under the Shared Savings Program (SSP).
-
001 / 001SSP – Diabetes: Hemoglobin A1c Poor Control (>9%)
This is an inverse measure, meaning lower performance rates reflect better clinical outcomes. This measure tracks the percentage of patients aged 18–75 with diabetes who had poor blood sugar control, defined as an HbA1c level greater than 9%. It reflects how well diabetes is being managed within a population. -
134 / 134SSP – Preventive Care and Screening: Screening for Depression and Follow-Up Plan
This measure captures whether patients aged 12 and older were screened for depression using a standardized tool and, if positive, whether an appropriate follow-up plan was documented. -
236 / 236SSP – Controlling High Blood Pressure
This measure looks at the percentage of patients aged 18–85 with a diagnosis of hypertension whose blood pressure was adequately controlled (i.e., <140/90 mmHg) during the measurement period.
The performance data across multiple APM entities reveals several important trends:
-
Blood pressure control (Measure 236/236SSP) consistently shows the highest average performance across both CQMs and eCQMs, with averages exceeding 70% and relatively narrow performance ranges. This suggests that APM participants are doing a strong job managing hypertension at the population level, likely benefiting from mature care protocols and better integration with primary care workflows.
-
Depression screening and follow-up (Measure 134/134SSP) shows considerably more variability across both reporting methods. While some organizations achieved performance rates above 60%, others fell well below 10%, particularly in eCQM submissions. This wide range may reflect challenges in documentation, workflow integration, or follow-up tracking, highlighting an area where additional support or quality improvement could drive more consistent performance.
-
Diabetes control (Measure 001/001SSP)—as an inverse measure—showed stronger results among entities using CQMs (with lower percentages indicating better control). However, performance varied significantly, with some APMs reporting over 50% of patients with poorly controlled diabetes.
One contributing factor is that point-of-care HbA1c testing results are often not fully integrated into EHR systems, especially in practices relying on rapid, in-office testing devices. When these results are not captured in structured EHR fields, they are excluded from eCQM calculations—leading to artificially inflated rates of poor control. Ensuring consistent capture and integration of A1c results, regardless of collection method, is crucial to improving both performance accuracy and patient outcomes. -
Additionally, CQMs generally demonstrated more consistent results than eCQMs, especially for Measures 134 and 001. This may reflect challenges in data completeness and mapping on the eCQM side.
In summary, while many APMs are excelling in hypertension management, challenges persist in behavioral health screening and diabetes control. Improving EHR workflows, integrating point-of-care data, and enhancing follow-up care can help close these gaps and ensure high-quality care delivery across value-based care models.
Why MDinteractive?
1. Data Aggregation Across Multiple EHRs
We support the collection and aggregation of data from multiple EHR systems, regardless of vendor, to meet the 75% data completeness threshold. Our tools normalize and validate data to ensure accuracy before submission.
2. Measure Performance Insight
Our analytics provide real-time performance dashboards, enabling ACOs to track progress on quality measures throughout the year. This allows organizations to make proactive decisions and close care gaps in real time.
3. Expert Guidance
With deep experience navigating CMS’s complex and evolving regulatory requirements, our team offers hands-on consulting and audit support to ensure compliant and high-quality submissions.
4. Secure and Scalable Platform
Designed to manage the complexities of large-scale ACO submissions, our secure platform ensures HIPAA-compliant data handling and seamless coordination across hundreds or even thousands of clinicians.
Preparing for the Future of Quality Reporting
As CMS continues to refine its quality reporting programs, now is the time for ACOs to strengthen their infrastructure and partnerships. The future points toward greater interoperability, all-payer data integration, and more stringent performance thresholds.
At MDinteractive, we are not just a vendor—we’re your strategic ally in delivering high-quality, value-based care.
Interested in learning how MDinteractive can streamline your ACO's quality reporting?
Reach out to us today to schedule a personalized consultation.
Leave a comment