During 2025, all Shared Savings Program ACOs will be required to report the APP Plus quality measure set, which includes four clinical quality measures, the CAHPS survey, and the readmission measure. CMS has published a Fact Sheet that outlines how ACOs can earn shared savings, but translating those rules into practice can be challenging. In practical terms, the ability to earn shared savings—or avoid financial losses—will depend on the reporting pathway you choose:
-
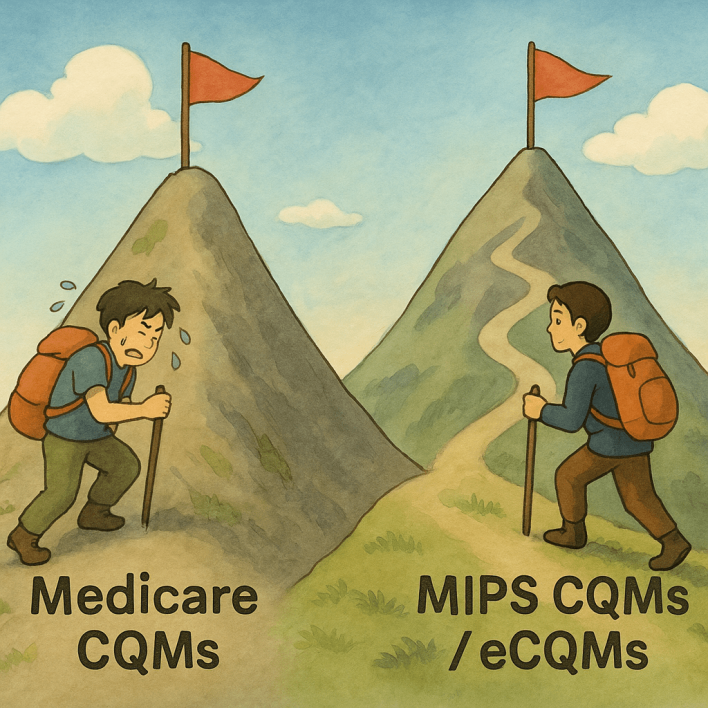
For eCQMs or MIPS CQMs: You can qualify for maximum shared savings by achieving ≤ 90% on A1c poor control and ≥ 65% on BP control.
-
For Medicare CQMs: You are considered in the 'safety zone' if you meet ≥ 67% on three quality measures, ≤ 34% on the inverse A1c measure, and score at least 7.67 points on both the CAHPS survey and the readmission measure.
| 2025 Quality Performance Standards Summary | ||
|---|---|---|
| Pathway | What you must clear | What you earn |
| Standard Quality Performance Standard (All ACOs) |
Achieve a health equity adjusted quality performance score ≥ 76.70 (40th percentile MIPS Quality performance category score, excluding facility-based entities) |
Maximum shared-savings rate and reduced downside risk |
| Standard Quality Performance Standard (For ACOs reporting all 4 eCQMs/MIPS CQMs with completeness) |
• Achieve a quality score ≥ 10th percentile on ≥ 1 of the 3 outcome measures • AND a score ≥ 40th percentile on ≥ 1 of the 5 remaining APP Plus measures |
Maximum shared-savings rate and reduced downside risk |
| Standard Quality Performance Standard (First year ACOs) |
Meet MIPS data completeness on 4 APP Plus CQMs + receive a MIPS Quality score + administer the CAHPS for MIPS Survey |
Maximum shared-savings rate and reduced downside risk |
| Alternative Quality Performance Standard (All ACOs) |
Achieve a quality score ≥ 10th percentile on ≥ 1 of the 3 outcome measures (reporting via APP using any combination of eCQM/MIPS CQM/Medicare CQM) |
Shared savings at a reduced rate scaled by health equity adjusted score; scaled shared losses for ENHANCED ACOs |
Everything below spells out what the Standard Quality Performance Standard means—measure by measure—for eCQMs, MIPS CQMs, and Medicare CQMs.
1 · eCQMs (all‑payer)
1.1 40th Percentile Threshold
-
Target: Average ≥ 7.67 points per measure (Decile 7) to reach the composite 76.70 once CAHPS and Hospital-Wide All-Cause Unplanned Readmission Measure (HWR) are factored in.
| 2025 Thresholds to Earn 7.67 Points by Measure | |||
|---|---|---|---|
| Quality ID | Measure | Inverse? | Performance Rate to earn 7.67 pts |
| 001 | HbA1c Poor Control > 9 % | Yes | ≤ 24.51% poor control |
| 112 | Breast‑Cancer Screening | No | ≥ 71.67 % screening |
| 134 | Depression Screening & Plan | No | ≥ 67.01% screening |
| 236 | Controlling High Blood Pressure | No | ≥ 74.20% BP control |
| 321 | CAHPS for MIPS | n/a | 2025 deciles released post‑performance year |
| 479 | 30‑Day All‑Cause Readmission | n/a | 2025 deciles released post‑performance year |
-
Action: Run quarterly test submissions out of your EHR and watch the decile scores; adjust workflows until each measure sits in Decile 7 or higher.
Benchmarks for eCQMs are historical and usually shift only 1‑2 percentage points year‑to‑year.
1.2 10/40 rule: 1 outcome ≥10th, 1 other ≥40th percentile
Official 2025 eCQM benchmarks identify the exact cut‑points you must hit on at least two measures—a qualifying outcome (≥10th pct) and any other measure (≥40th pct):
| 2025 Quality Measure Cut-Points and Scoring | ||||
|---|---|---|---|---|
| Quality ID | Measure | Inverse? | 2025 cut‑point you must hit | Points earned |
| 001 | Diabetes: HbA1c Poor Control > 9 % | Yes | ≤ 94.35 % poor‑control rate (10th pct) | 2 pts |
| 236 | Controlling High Blood Pressure | No | ≥ 65.32 % BP‑control rate (40th pct) | 5 pts |
TIP: By meeting just two targets — a performance rate of ≤ 94.35% on A1c poor control and ≥ 65.32% on BP control — and ensuring data completeness across all four eCQMs, the ACO can qualify for the maximum shared savings rate.
2 · MIPS CQMs (all-payer)
2.1 40th Percentile Threshold
-
Same math as eCQMs: shoot for ≥7.67 points per measure.
| 2025 Thresholds to Earn 7.67 Points by Measure | |||
|---|---|---|---|
| Quality ID | Measure | Inverse? | Performance Rate to earn 7.67 pts |
| 001 | HbA1c Poor Control > 9 % | Yes | ≤ 33.93% poor control |
| 112 | Breast‑Cancer Screening | No | ≥ 85.76 % screening |
| 134 | Depression Screening & Plan | No | 100% screening |
| 236 | Controlling High Blood Pressure | No | ≥ 66.7% BP control |
| 321 | CAHPS for MIPS | n/a | 2025 deciles released post‑performance year |
| 479 | 30‑Day All‑Cause Readmission | n/a | 2025 deciles released post‑performance year |
2.2 10/40 rule: 1 outcome ≥10th, 1 other ≥40th percentile
Official 2025 MIPS CQM benchmarks identify the exact cut‑points you must hit on at least two measures—a qualifying outcome (≥10th pct) and any other measure (≥40th pct):
| Practical 2025 Quality Targets and Rule Alignment | |||||
|---|---|---|---|---|---|
| Quality ID | Measure | Inverse? | Practical 2025 target | Points | Which rule it satisfies |
| 001 | HbA1c Poor Control > 9 % | Yes | ≤ 90 % poor‑control rate | 2 pts | ≥10th‑pct outcome |
| 236 | Controlling High Blood Pressure | No | ≥ 40 % BP‑control rate | 5 pts | ≥40th‑pct other |
TIP: Achieving just these two targets — a performance rate of ≤ 90% on A1c poor control and ≥ 40% on BP control — while meeting data completeness on all four MIPS CQMs, enables the ACO to earn the maximum shared savings rate
3 · Medicare CQMs
40th Percentile Threshold (Only Path for Medicare CQMs)
Medicare CQMs are scored with flat (static) benchmarks for 2025. The goal under the standard pathway is to keep each measure at ≥7.67 points.
| 2025 Thresholds to Earn 7.67 Points by Measure | |||
|---|---|---|---|
| Quality ID | Measure | Inverse? | Performance Rate to earn 7.67 pts |
| 001SSP | HbA1c Poor Control > 9 % | Yes | ≤ 33.93% poor control |
| 112SSP | Breast‑Cancer Screening | No | ≥ 66.7 % screening |
| 134SSP | Depression Screening & Plan | No | ≥ 66.7% screening |
| 236SSP | Controlling High Blood Pressure | No | ≥ 66.7% BP control |
| 321 | CAHPS for MIPS | n/a | 2025 deciles released post‑performance year |
| 479 | 30‑Day All‑Cause Readmission | n/a | 2025 deciles released post‑performance year |
Operational checklist
-
Mid‑year mock submission – Verify decile scores in your EHR/registry.
-
Focus resources – If the quality performance score of ≥ 76.70 for Medicare CQMs seems out of reach, consider switching to MIPS CQMs or eCQMs reporting as soon as possible — MDinteractive can help you evaluate and report across all these options. Schedule an MDinteractive ACO Reporting Demo to get started.
-
Watch inverse logic – Lower is better on the A1c measure #1; double‑check that dashboards are interpreting it correctly.
-
Document everything – Numerator/denominator logic and exclusion handling.
Key take‑aways
-
Under eCQMs or MIPS CQMs, achieving ≤ 90% on A1c poor control and ≥ 65% on BP control — or scoring an outcome measure in Decile 2 plus any other measure in Decile 5 — enables the ACO to qualify for maximum shared savings
-
For Medicare CQMs, an ACO can achieve a quality performance score of ≥ 76.70 by reaching ≥ 67% on three quality measures, ≤ 34% on the inverse A1c measure, and scoring at least 7.67 points on both the CAHPS survey and the readmission measure.
-
If the performance targets for Medicare CQMs seem out of reach, switch to MIPS CQMs or eCQMs — and ensure that at least one outcome measure is at the 10th percentile and another measure at the 40th percentile.
-
Nail these numbers early; the rest of APP Plus becomes a formality.
-
Take the next step — schedule your ACO reporting demo with MDinteractive.
Leave a comment