
On August 12, 2024, the Centers for Medicare & Medicaid Services (CMS) released the Final Performance Feedback for the 2023 Merit-based Incentive Payment System (MIPS) performance period. Reviewing your performance feedback now is vital to understanding your final MIPS scores and payment adjustment details. If you suspect an error in the calculation of your MIPS payment adjustment, you have until 8 p.m. ET on October 11, 2024, to request a targeted review. This article outlines step-by-step instructions for accessing your performance feedback, evaluating your payment adjustment status—positive, negative, or neutral—and filing a targeted review if necessary.
Information Available in the Final Performance Feedback
The 2023 MIPS Final Performance Feedback reflects all of the data submitted or calculated for an individual clinician, group, or APM Entity participating in MIPS. It includes final MIPS scores and payment adjustment information associated with the 2023 reporting period based on reporting traditional MIPS, a MIPS Value Pathway (MVP), or the APM Performance Pathway (APP).
Here’s a breakdown of what’s included in the Final Performance Feedback:
- Final score
- Performance category-level scores and weights
- Bonus points and improvement scoring
- Measure-level performance data and scores
- Activity-level scores
- Payment adjustment information
- Supplemental reports for administrative claims quality and cost measures
- Comparative quality and cost feedback (MVP reporting only)
How to Access Your MIPS Final Score and Payment Adjustment Details
Clinicians and authorized representatives of practices and APM Entities (including Shared Savings Program Accountable Care Organizations [ACOs]), can access the Final Performance Feedback by logging into the Quality Payment Program website and clicking "View PY 2023 Final Performance Feedback” on the home page.
MDinteractive can assist clinicians with accessing their performance feedback and interpreting the results if they have an MDinteractive account.
- If you previously permitted us to access your reports, we have uploaded them to your MDinteractive account. The reports can be accessed by clicking the green “QPP Performance Feedback” icon on your MIPS dashboard and selecting “2023 QPP Feedback” to view your 2023 scores and payment adjustment.
- If you have not already given us access, please follow the steps below:
- First, create a QPP Harp Account if you still need to do so.
- Next, log into your MDinteractive account at www.mdinteractive.com
- Complete the steps by clicking the blue "QPP Performance Feedback" icon on your dashboard.
APMs
APM Entity representatives who hold the Staff User or Security Official role have the ability to review MIPS final scores for their respective APM Entity. Additionally, QPP Security Officials or QPP Staff User contacts within the Medicare Shared Savings Program Accountable Care Organization (ACO) can access the ACO’s MIPS final score by logging into the QPP website using their ACO Management System (ACO-MS) credentials.
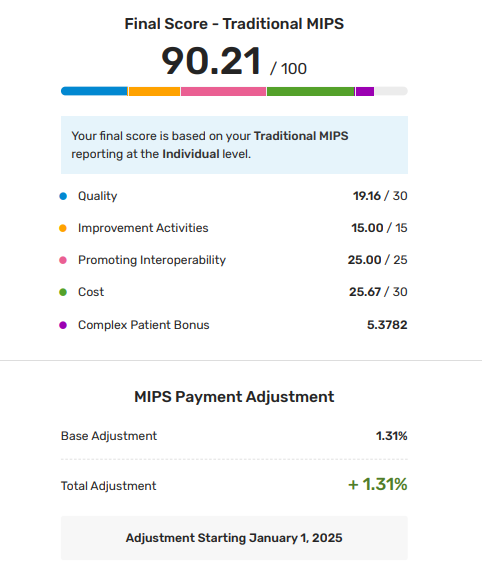
What Makes Up the Final MIPS Score
The final MIPS score is the sum of the MIPS performance category scores and any points awarded for the complex patient bonus. CMS assigns you the highest possible score based on your Tax Identification Number (TIN) and individual National Provider Identification (NPI) combination if you participated in MIPS in multiple ways (e.g., for example, your practice reported traditional MIPS at the group level and the clinician also reported an MVP as an individual — we’ll assign the highest score that could be attributed to the clinician under that TIN/NPI combination.
MIPS Cost Category
For the 2023 reporting year, the Cost category was worth 30% of your final MIPS score as long as you could be scored on at least one Cost measure. If there are no Cost measure details and a score of “N/A” in your Performance Feedback then the case minimum requirements were not met for any cost measures and the weight for this performance category was reallocated to another category. If you were approved for reweighting in this performance category you can still access measure-level and patient-level feedback if the case minimum was met for at least one Cost measure.
Note CMS excluded the Simple Pneumonia with Hospitalization measure for all MIPS eligible clinicians. The measure wasn’t included in CMS’s calculation of MIPS any scores under the Cost category for the 2023 performance period.
Patient-Level Reports
Patient-level reports offer detailed information about the patients included in the calculation of Cost and Quality administrative claims measures, along with insights into how these measures are scored. These reports are available if you meet the case minimum for the measures.
Complex Patient Bonus
The complex patient bonus is limited to MIPS eligible clinicians, groups, and APM Entities with at least one risk indicator (either average Hierarchical Condition Categories [HCC] risk score or dual eligibility ratio) at or above the median risk indicator calculated for all MIPS eligible clinicians, groups, and APM Entities from the prior performance year.
Improvement Scoring
Eligible clinicians can earn up to 10 additional percentage points in the Quality performance category based on improvement from the previous year. In the Cost performance category, up to 1 additional percentage point can be earned depending on the rate of year-over-year improvement.
Facility-Based Scoring
If your quality and cost scores are derived from facility-based scoring, you won’t see measure details. Instead, you’ll see your facility’s Hospital VBP Program score and associated percentile
and the MIPS equivalent (unweighted) quality score based on the Hospital VBP Program
score’s percentile. The MIPS equivalent score is multiplied by the category weight to arrive
at the quality points contributing to your final score.
2025 Payment Adjustments
Your final score was compared to performance thresholds to determine whether you’ll receive a positive, negative, or neutral adjustment to payments for the covered professional services you furnish in the 2025 MIPS payment year. Payment adjustment factors are assigned on a linear sliding scale:
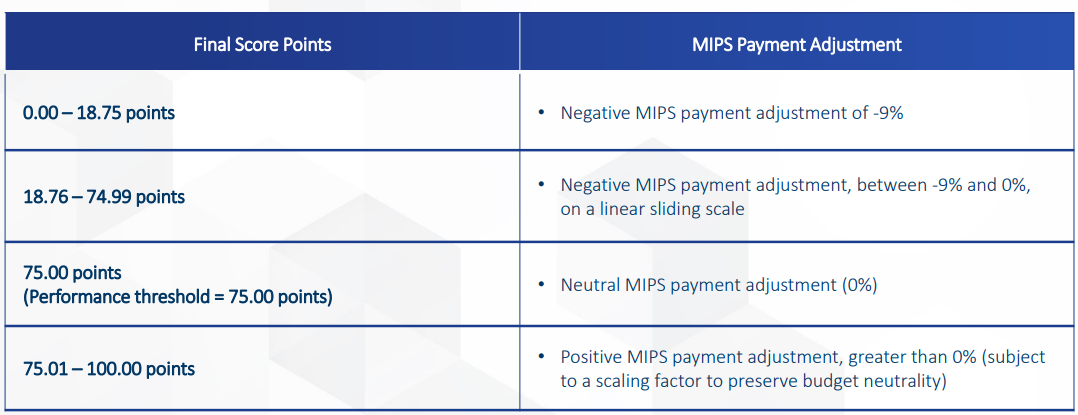
As a reminder, MIPS is required by law to be budget neutral, meaning projected negative adjustments must balance with projected positive adjustments. Positive payment adjustments are influenced by the performance threshold and the distribution of final scores compared to this threshold each year.
If a MIPS payment adjustment is applied to a payment made to a MIPS eligible clinician, the following codes will be displayed on the remittance advice (RA) documents:
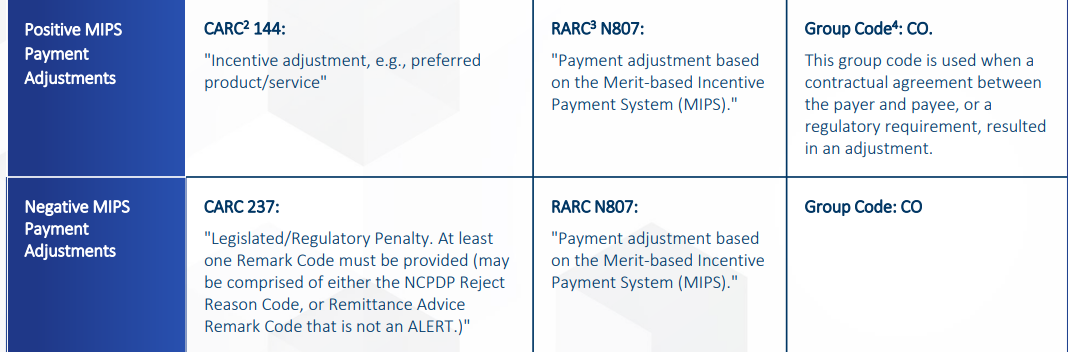
The 2025 MIPS payment adjustments vary between -9% and +2.15%. A perfect score of 100 MIPS points would result in a positive payment adjustment of +2.15%. Federal law requires CMS to implement MIPS payment adjustments in a budget-neutral manner.
The table below provides examples of different 2023 MIPS final scores and their estimated payment adjustments:
| 2023 MIPS Final Score | 2025 Payment Adjustment Estimates |
|---|---|
| 100 | +2.15% |
| 90 | + 1.31% |
| 80 | + 0.43% |
| 75 | 0 |
| 70 | - 0.57% |
| 60 | - 1.70% |
| 50 | - 3.00% |
| 40 | - 4.22% |
| 0 | -9% |
How to File a Targeted Review
Carefully review your performance feedback now to determine if a targeted review should be filed. If you don’t agree with your final MIPS score or the payment adjustment information, there is a limited window of time to appeal the decision via a targeted review process.
A targeted review can be requested via a QPP account until 8 p.m. ET on October 11, 2023. It should be requested at the same level as you reported MIPS (individual or group). CMS suggests requesting a targeted review as soon as possible if you identify an error with your MIPS final performance feedback and MIPS payment adjustment factor(s). This will help
ensure that the correct payment adjustment is applied to your claims from the start of the 2025 payment year.
CMS lists the following examples of circumstances for which you may wish to request a
targeted review:
- Your performance data was submitted under the incorrect TIN or NPI.
- You qualified for performance category reweighting because of a special status designation, Promoting Interoperability Hardship Exception, or Extreme and Uncontrollable Circumstances Exception that was incorrectly applied.
As a reminder, once the targeted review deadline passes, you will no longer have a way to dispute your scores. This is why it is important to review your performance feedback reports as soon as they are available.
The QPP Service Center is open Monday-Friday from 8 a.m. - 8 p.m. EST at 1-866-288-8292 or by e-mail at QPP@cms.hhs.gov.
Any Questions?
Check your 2023 MIPS final scores and payment adjustments now and file a targeted review before the CMS deadline if you believe an error was made in your payment adjustment calculation. MDinteractive can help you access your performance feedback or interpret the results. MIPS reporting is getting tougher each year, so early planning is critical for MIPS success. If you have not yet started your 2024 MIPS reporting, log in to your MDinteractive account now to complete your 2024 MIPS reporting plans and begin your reporting.
Leave a comment