
The MIPS Promoting Interoperability category focuses on the use of certified electronic health record technology to enhance patient access to their medical records and promote the transfer of data among healthcare clinicians. In this updated blog, we'll explore the latest PI reporting requirements for 2024 and offer tips to enhance reporting success.
2024 Promoting Interoperability (PI) Updates
In 2024, the MIPS Promoting Interoperability performance category has undergone several key changes:
180-Day Minimum Reporting Period
Beginning in 2024 the minimum performance period for the PI category is increased to 180 continuous days within the calendar year (up from a minimum of 90 days in 2023). This means the last 180-day performance period begins on July 5, 2024.
Updated CEHRT Definition
Reporting the PI category requires the use of a Certified Electronic Health Record Technology (CEHRT). The definition of CEHRT has been revised to conform with the regulations set forth by the Office of the National Coordinator for Health IT (ONC), which have shifted away from the use of the "edition" framework for certification criteria. Mentions of the "2015 Edition health IT certification criteria" will now be replaced with "ONC health IT certification criteria.
Clinicians can confirm if their EHR system and modules are certified for the MIPS PI category by checking the Certified Health IT Product List (CHPL) on the ONC website.
Annual Assessment of the High Priority Guide is Required
Clinicians must conduct an annual self-assessment using the High Priority Practices Guide (a part of the SAFER Guides), within the calendar year of the performance period. A “yes” response is required. A “no” response will no longer satisfy this measure. Below are some tips to effectively complete the annual self-assessment:
- Review the recommended practices at the beginning of the Guide and mark the checkboxes next to each practice based on your implementation status (fully, partially, or not implemented).
- Refer to the detailed worksheets that follow the checklist section for guidance on implementing each practice. These worksheets provide examples, potential sources of information to help assess your practices, and spaces for noting any follow-up actions needed.
More information can be found on the SAFER Guides webpage on HealthIT.gov.
Updates to the Query of Prescription Drug Monitoring Program (PDMP) Measure
The current exclusion for the Query of Prescription Drug Monitoring Program (PDMP) Measure was modified to accommodate clinicians who don’t electronically prescribe any Schedule II opioids and Schedule III and IV drugs during the performance period.
PI Reweighting Changes
CMS discontinued automatic reweighting for the following clinician types beginning in 2024:
- Physical therapists
- Occupational therapists
- Qualified speech-language pathologists
- Clinical psychologists
- Registered dietitians or nutrition professionals
Automatic reweighting will continue for the following clinician types in the 2024 performance period:
- Clinical social workers
- ASC-based clinicians and groups
- Hospital-based clinicians and groups
- Non-patient facing clinicians and groups
- Clinicians in a small practice (15 or less)
*Clinicians that do not qualify for PI to be automatically reweighted can apply to CMS to obtain an exemption from the PI category due to a “significant hardship”. The 2024 QPP Exception applications are open until December 31, 2024, at 8 p.m. ET. The Hardship exception can be submitted by individual clinicians, groups, or virtual groups if they face issues like decertified EHR technology, insufficient internet connectivity, extreme circumstances like disasters, or lack of control over CEHRT. Approval of this application exempts clinicians from reporting data for this category.
PI Basics
What are the PI Measures?
The PI category is divided into a series of objectives and measures. The four objectives focus on the following topics:
- e-Prescribing
- Health Information Exchange (HIE)
- Provider to Patient Exchange
- Public Health and Clinical Data Exchange
Within each of the objectives are required measures and optional measures. Data must be submitted for all required PI measures from each of the objectives (unless an exclusion can be claimed) for the same 180 continuous days (or more). The table below details each of the measures, potential scores, and any applicable exclusions.
| 2023 PI Objectives and Measures | ||||
|---|---|---|---|---|
| Objectives | Measures | Reporting Requirements | Available Points | Exclusions |
| e-Prescribing | e-Prescribing | Required; Numerator/ Denominator | 1-10 points | Writes fewer than 100 e-prescriptions during the performance period. |
| Query of Prescription Drug Monitoring Program (PDMP) | Required; Yes/No |
10 points | Unable to e-prescribe Schedule II opioids and Schedule III and IV drugs in accordance with applicable law during the performance period; OR does not electronically prescribe any Schedule II opioids or Schedule III or IV drugs during the performance period.* |
|
| Health Information Exchange (Choose 1 of the 3 options) | Option 1 | |||
| Support Electronic Referral Loops by Sending Health Information |
Required (unless Option 2 or 3 is reported); Numerator/ Denominator |
1-15 points | Transfers a patient to another setting or refers patients fewer than 100 times during the performance period. | |
| Support Electronic Referral Loops by Receiving and Reconciling Health Information | 1-15 points | Receives fewer than 100 transitions or referrals, or has fewer than 100 encounters with patients never before encountered during the performance period. | ||
| Option 2 | ||||
| HIE Bi-Directional Exchange |
Required (unless Option 1 or 3 reported); Yes/No |
30 points | No exclusion available. | |
| Option 3 | ||||
| Enabling Exchange under the Trusted Exchange Framework and Common Agreement (TEFCA) |
Required (unless option 1 Yes/No |
30 points | No exclusion available. | |
| Provider to Patient Exchange | Provide Patients Electronic Access to Their Health Information | Required; Numerator/ Denominator |
1-25 points | No exclusion available. |
| Public Health and Clinical Data Exchange* |
Report the 2 required measures: |
Required; Yes/No (must also submit level of active engagement) |
25 points for the entire objective |
Exclusion for Immunization Registry Reporting: Does not administer any immunizations; OR operates in a jurisdiction with no immunization registry; OR operates in a jurisdiction where no immunization registry has declared readiness to receive immunization data as of 6 months prior to the start of Exclusion for Electronic Case Reporting: Does not treat or diagnose any reportable diseases for which |
| Optional; Yes/No |
5 bonus points (whether reporting 1, 2, or all 3 optional measures |
No exclusion available. | ||
*Note: If a clinician reports MIPS to a registry it does not count towards the Public Health and Clinical Data Exchange objective. Click here for more information on how to engage with MDinteractive’s Clinical Data Registry to ensure PI bonus points can be earned for this measure.
In addition to reporting on the above PI measures, you must also provide your EHR’s CMS Certification ID code and attest to the following statements with a 'yes' response when reporting the PI category:
- The Actions to Limit or Restrict Compatibility or Interoperability of CEHRT Attestation.
- The Office of the National Coordinator for Health Information Technology (ONC) Direct Review Attestation.
- The Security Risk Analysis Measure.
- The Safety Assurance Factors for EHR Resilience (SAFER) Guides Measure.
Remember, if you fail to report on a required attestation or measure (or claim an applicable exclusion) you will receive a score of zero for the PI category.
How is PI Scored?
The PI score is the sum of points earned for the submitted measures multiplied by the 25% PI category weight. Each PI measure is scored based on the clinician or group’s performance on the measure (e.g., the numerator/denominator submitted or answering “yes,” if applicable). A maximum score of up to 105 points can be earned in this category, but the score is capped at 100. If you claim an exclusion for a measure, the measure’s points are reallocated to a different measure.
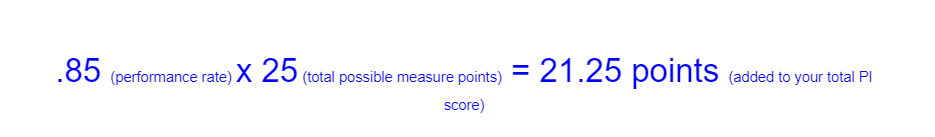
Performance Score Illustration:
A numerator/denominator of 170/200 for the Provider to Patient Exchange (worth up to 25 points) would have a performance rate of 85%. The points for this measure would be calculated as follows:
While most of the measures have an exclusion available, it’s important to remember that when an exclusion is claimed, the points for the measure will be redistributed to another measure or measures.
PI Score Illustration:
Here’s an example of how the total PI score is calculated if a clinician earned 75 PI points (total points from all objectives/measures):
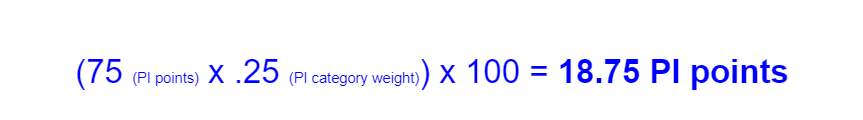
Important: Since scoring is based on a clinician or group’s performance for each measure, earning the full 25 points for PI in the final MIPS score could be more difficult. And, if a required measure, such as Provider to Patient Exchange, is not reported, or an exclusion for a required measure is not claimed, the clinician or group will receive a total score of 0 for the PI performance category. Clinicians should pay close attention to their performance on the measures and make improvements where necessary to maximize their PI score and Medicare payment adjustments.
APMS
When participating in MIPS at the APM Entity level, APM Entities can choose to report PI data at the APM Entity level. However, APM Entities still have the option to report this performance category at the individual and group levels.
PI Checklist
Below are a few tips to help you get started with your PI reporting:
- Understand the Requirements: Confirm if you are required to report the PI category. Familiarize yourself with the PI objectives and measures and read the CMS guidelines to ensure you have a clear understanding of what's expected.
- Use Certified EHR Technology (CEHRT): Confirm your EHR is certified. Check your certification status here.
- Review Your Progress: Keep track of your performance throughout the reporting period to ensure you're on track to meet your PI goals. Run a trial report in your EHR of the 2024 PI measures and review your performance for each measure. View the 2024 measures here. Important measures to test:
- Provide Patients Electronic Access to Their Health Information
- Support Electronic Referral Loops by Sending Health Information
- Support Electronic Referral Loops by Receiving and Reconciling Health Information
- Provide Patients Electronic Access to Their Health Information
- Check Your Reporting Period: The PI reporting period must be a minimum of 180 continuous days in 2024, but can be longer. CEHRT functionality that meets ONC’s certification criteria must be in place by July 5th, 2024. The EHR must be certified by ONC to the certification criteria by December 31st, 2024.
- Maintain Documentation: Supporting documentation does not need to be included with your PI attestation, however, you must keep documentation supporting the PI data you have reported for 6 years after submission in the event of an audit.
Leave a comment