
Navigating the complexities of the Merit-based Incentive Payment System (MIPS) can be challenging, but understanding the Quality category is crucial for clinicians aiming to optimize their performance scores. As we approach the midpoint of the 2024 MIPS reporting year, clinicians should already be actively collecting and reporting data on their Quality measures. The Centers for Medicare and Medicaid Services (CMS) has announced that it is not accepting hardship applications due to COVID-19 for the 2024 performance year, so some clinicians may find themselves reporting MIPS for the first time in several years and discover that a lot has changed. This article will provide an in-depth overview of the 2024 Quality reporting requirements, changes to quality measures, and tips for selecting the best measures for one's practice.
The MIPS Quality Category
The MIPS Quality category assesses clinicians and groups on healthcare quality measures, including processes, outcomes, and patient experiences. Quality is weighted differently based on the size of the practice:
- 30% of the total MIPS score for large practices (16 or more NPIs).
- 40% of the total MIPS score for small practices (15 or fewer NPIs) that do not report the Promoting Interoperability (PI) category.
*MIPS category weights may change based on special statuses, exception applications, or reweighting of other performance categories.
What are the MIPS Quality Category Reporting Requirements?
The Quality performance category has a 12-month performance period (January 1 – December 31, 2024), so data must be collected for each measure for the full calendar year. Clinicians will:
- Select six measures (including an outcome or a high-priority measure) or a specialty measure set or a MIPS Value Pathway (MVP). Note: If reporting an MVP four quality measures are selected from the list of measures in the MVP (one must be an outcome or a high-priority measure).
- Report at least 75% (up from 70% in 2023) of eligible encounters for all insurances. This data completeness threshold will remain at 75% for the 2025 and 2026 performance periods.
In certain cases, clinicians can report less than six measures through the Eligible Measures Applicability (EMA) Process. Under EMA, for example, an anesthesiologist may only need to report four quality measures (404, 424, 430, and 463) with a registry. Some specialty measure sets may also have fewer than 6 measures to report. If reporting the Hospitalist Specialty measure set, for example, only 4 Quality measures must be reported (#5, #8, #47, and #130).
What Quality Measures are Available to Report in 2024?
A total of 198 quality measures are available for reporting this year. Clinicians should select quality measures that align with their practice, considering the type of care they offer and the clinical conditions they typically treat.
Explore the complete list of 2024 Quality measures or find measures specific to a specialty.
The 2024 Quality measure inventory reflects the following changes from the last reporting year:
- 11 new Quality measures
- Removal of 11 Quality measures
- Partial removal of three measures (retained for MVP use only)
- Substantive changes to 59 existing Quality measures
New measures available to report in 2024 are listed in the table below.
A list of measures that have been removed or partially removed is included in the table below.
| Removed Quality Measures | Collection Type |
|---|---|
| #14 Age-Related Macular Degeneration (AMD): Dilated Macular Examination | MIPS CQM |
| #93 Acute Otitis Externa (AOE): Systemic Antimicrobial Therapy – Avoidance of Inappropriate Use | MIPS CQM |
| #107 Adult Major Depressive Disorder (MDD): Suicide Risk Assessment | eCQM |
| #110 Preventive Care and Screening: Influenza Immunization | Medicare Part B Claims, eCQM, MIPS CQM |
| #111 Pneumococcal Vaccination Status for Older Adults | Medicare Part B Claims, eCQM, MIPS CQM |
| #138 Melanoma: Coordination of Care | MIPS CQM |
| #147 Nuclear Medicine: Correlation with Existing Imaging Studies for All Patients Undergoing Bone Scintigraphy | Medicare Part B Claims, MIPS CQM |
| #283 Dementia Associated Behavioral and Psychiatric Symptoms Screening and Management | MIPS CQM |
| #324 Cardiac Stress Imaging Not Meeting Appropriate Use Criteria: Testing in Asymptomatic, Low-Risk Patients | MIPS CQM |
| #391 Follow-Up After Hospitalization for Mental Illness (FUH) | MIPS CQM |
| #402 Tobacco Use and Help with Quitting Among Adolescents |
MIPS CQM |
| Quality Measures Removed from Traditional MIPS* (retained for MVPs only) |
Collection Type |
| #112: Breast Cancer Screening | Medicare Part B Claims, eCQM, MIPS CQM |
| #113: Colorectal Cancer Screening | Medicare Part B Claims, eCQM, MIPS CQM |
| #128: Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-up Plan | Medicare Part B Claims, eCQM, MIPS CQM |
Have There Been Any Changes to Existing Quality Measures?
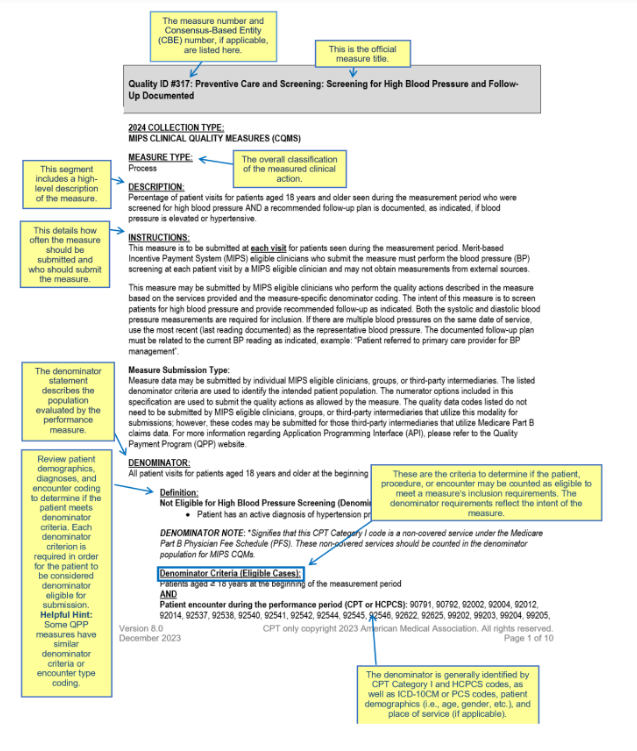
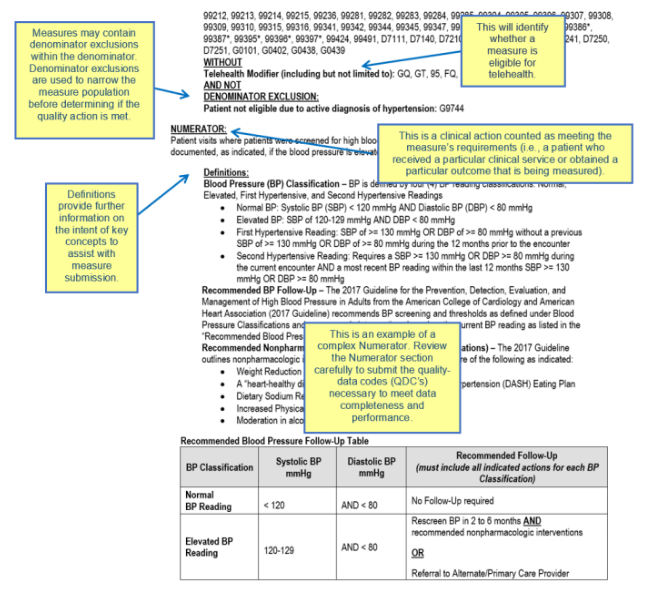
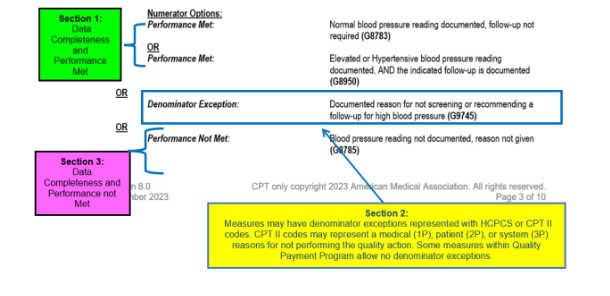
Every quality measure comes with its own set of specifications, which may also undergo changes from year to year. The individual measure specifications are detailed descriptions of the quality measures and include important instructions for reporting each measure, including:
- How frequently the measure should be reported (e.g., once per year or at “every” visit).
- The unique eligible population to report (denominator) based on billing codes, diagnosis codes, and other patient demographics (e.g., age, gender, etc.).
- How to comply with the measure (the defined quality actions) for the eligible population (numerator).
CMS made substantive changes to 59 quality measures for the 2024 performance year. Clinicians should carefully review the measure specifications to ensure they are reporting each measure correctly. The CMS diagram below explains how to read the CMS documentation for a Quality measure.
Below are a few examples of changes for some commonly reported measures.
- #052: Chronic Obstructive Pulmonary Disease (COPD): Long-Acting Inhaled Bronchodilator Therapy
- An additional submission was added for spirometry so the measure now has two performance rates.
- #134: Preventive Care and Screening: Screening for Depression and Follow-Up Plan
- The denominator exclusion of depression was removed.
- #141: Primary Open-Angle Glaucoma (POAG): Reduction of Intraocular Pressure (IOP) by 20% OR Documentation of a Plan of Care
- The 15% reduction was changed to 20% reduction in IOP from pre-intervention level.
- #226: Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- Age change from 18 to 12 years of age.
- #459: Back Pain After Lumbar Surgery and #461: Leg Pain After Lumbar Surgery
- Both measures now have two performance rates- discectomy/laminectomy and fusion.
- #487: Screening for Social Drivers of Health
- A denominator exception was added for “patient reason for not screening… (e.g., patient declined or other patient reasons).
How Are Quality Measures Scored?
CMS will score the top 6 Quality measures, including at least 1 Outcome or High Priority measure. The number of points awarded for a Quality measure will depend on various factors.
|
2024 Quality Measure Scoring Policies |
|
|---|---|
| 1-10 points |
Measures can generally earn between one and ten points based on a clinician or group’s performance if the measures have a benchmark, meet data completeness (75% of eligible cases reported), and meet case minimum requirements (at least 20 eligible cases for the year). * Note: Some “topped out” measures are capped at 7 points. |
| 7 points | New measures in their first year have a scoring floor of seven points.
|
| 5 points | New measures in their second year have a scoring floor of five points.
|
| 0 points | Measures will earn zero points if data completeness and case minimum requirements aren’t met, or if the measure has no benchmark (small practices will continue to earn three points).* |
*These scoring policies don’t apply to new measures during the first 2 performance
periods available for reporting.
How Do Benchmarks Impact Measure Scoring?
Quality measures are assessed against their benchmark to determine how many points the measure receives based on the clinician or group’s performance. Each measure has its own benchmark that is specific to the collection type: Qualified Clinical Data Registry (QCDR) measures, MIPS Clinical Quality Measures (MIPS CQMs)*, electronic CQMs (eCQMs), CMS Web Interface measures, the Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey, and Part B Claims measures. For quality measures with no historical benchmark, CMS may calculate a benchmark based on 2024 data post-submission if CMS collects sufficient data during the performance period.
A “topped out” measure is one where the national median performance rate is so high that there is no meaningful difference in performance between clinicians. Some topped out measures are capped at seven points (versus 10 points) and can make it harder to optimize Quality category scores.
Clinicians should closely examine the measure benchmarks to understand the scoring implications for the measures they plan to report. All 2024 measure benchmarks can be found here.
Tips for Selecting Measures
Here are some tips for clinicians to consider when selecting Quality measures to report in 2024:
- Review Measure Relevance: Assess the relevance of each measure to your practice and unique patient population. Focus on measures that align closely with your specialty and the services you provide.
- Prioritize High-Impact Measures: Identify measures that have a significant impact on patient outcomes and healthcare quality and that have high-scoring potential. You may want to consider reporting new measures introduced in 2024 that have a higher scoring floor.
- Consider Data Volume: Evaluate the feasibility of collecting and reporting data for each measure based on the CMS documentation, paying careful attention to the eligible population you must report and how frequently the measure must be reported. Choose measures that can be easily and reliably captured within your practice's workflow.
- Optimize Performance: Analyze your historical performance data to identify areas where you have excelled or areas that require improvement. Select measures that allow you to showcase your strengths or demonstrate progress in areas where you aim to enhance performance.
- Stay Informed: Keep up with updates and changes to MIPS measures and reporting requirements. Regularly review guidance from CMS to ensure you are aware of any modifications or new measures introduced.
- Plan for Long-Term Success: Look beyond the current reporting year and consider measures that align with your long-term quality improvement goals. Select measures that can help drive meaningful change and promote continuous enhancement of patient care.
Selecting the right Quality measures appropriate for your practice is the first step toward successful MIPS reporting. MDinteractive provides many resources to help you develop an effective MIPS reporting plan, including guidance on measure selection and suggestions to simplify your data collection and reporting efforts.
Leave a comment