
CMS has released the 2018 MIPS performance feedback. The feedback will include a clinician or group’s performance category scores, final MIPS score and payment adjustment information. Any upward, downward or neutral payment adjustment will apply to the clinician or group’s 2020 Medicare Part B payments for covered professional services. CMS is allowing a Targeted Review to be requested until September 30, 2019.
Accessing Your 2018 MIPS Performance Feedback
The 2018 MIPS performance feedback is available via the Quality Payment Program (QPP) website. If you would like assistance in accessing your feedback reports or interpreting the results, MDinteractive can help. Just follow these simple instructions:
- Log into your MDinteractive account.
- Set up your dashboard if you haven’t already done so by entering your NPI and TIN (or just the TIN if you reported MIPS as a group). If you reported with MDinteractive in the past, you might see an option to import your providers from previous years so you don’t have to re-enter your NPIs/TINs.
- Click on the blue "QPP Performance Feedback" icon under the "Final Score" column of your dashboard. You will be directed to follow a few steps to give us permission to access the reports.
Once we have your reports, we will upload them to the File Storage area of your MDinteractive account and send you an email. If you have questions about the data, or need guidance on how to improve your future scores, you can contact one of our MIPS specialists for assistance.
Making Sense of Your MIPS Score
Performance Categories
Your 2018 MIPS final score will be between 0 and 100 points. The score is based on your performance in 4 MIPS categories, with each performance category having a different weight:
- Quality (50%)
- Promoting Interoperability (25%)
- Improvement Activities (15%)
- Cost (10%)
Remember, the weights can vary in some circumstances if you met the criteria to qualify for reweighting (e.g., hospital-based MIPS clinicians, non-patient facing MIPS clinicians, approval of a hardship application, extreme and uncontrollable circumstances, etc.).
Bonuses
Your MIPS final score may also include additional awarded bonus points, such as a small practice status or complex patient bonus. Clinicians and groups who were also eligible for MIPS in 2017 and submitted Quality data could be eligible for an additional Quality Improvement Bonus.
How Your MIPS Payment Adjustment is Calculated
If you were eligible for MIPS last year, you had to earn at least 15 MIPS points to avoid a penalty in 2020. If you earned over 15 MIPS points, you are eligible for a positive adjustment (the more points you earn, the higher possible adjustment you will receive). Earning 70 or more points would result in an exceptional performance bonus.
The 2020 MIPS payment adjustments vary between -5% and 1.68%. Since federal law requires CMS to implement MIPS payment adjustments in a budget-neutral manner, the highest upward adjustment is below +5%.
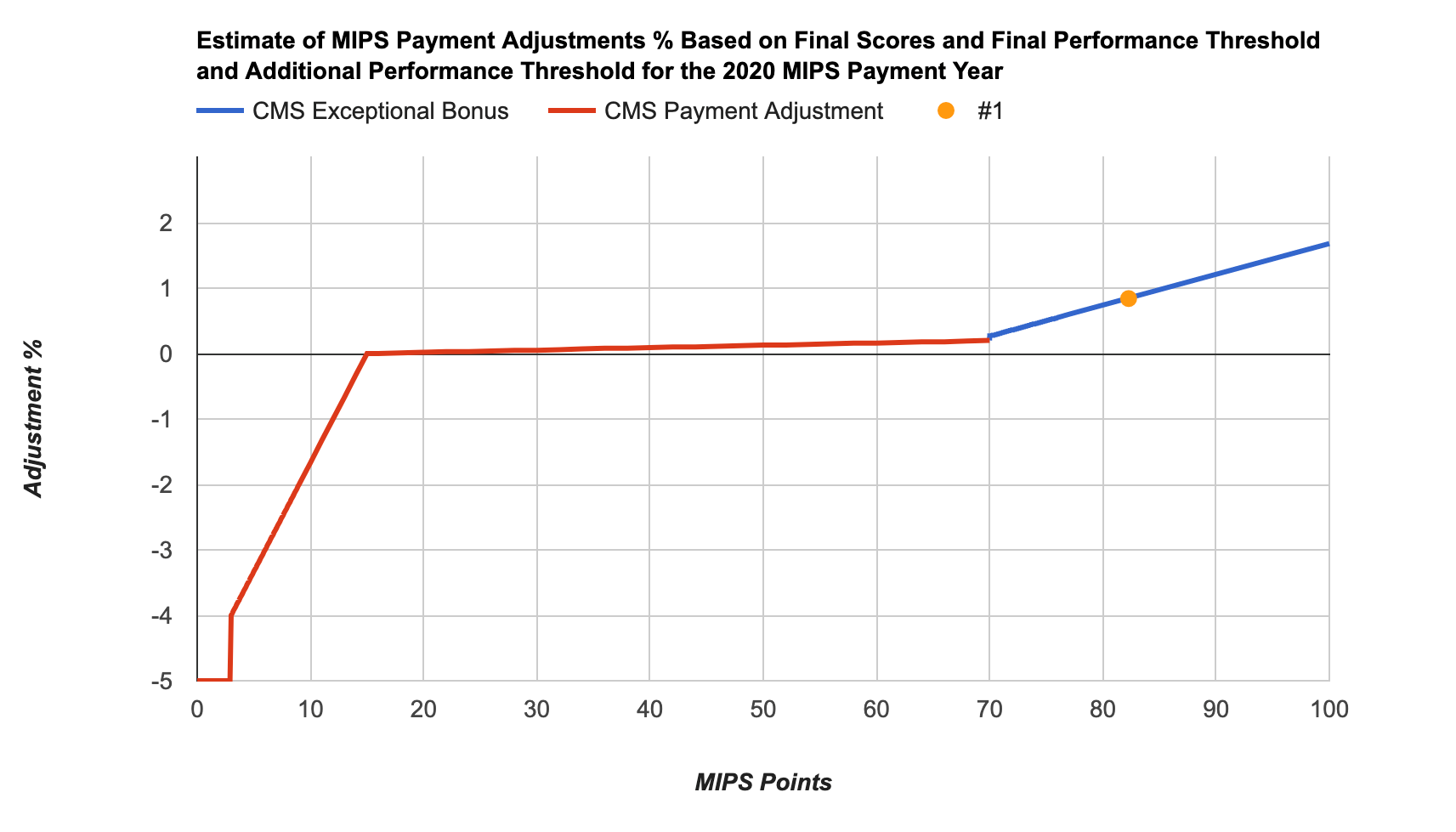
Below are some examples of MIPS scores and matching payment adjustments:
| 2018 MIPS Final Score | 2020 Payment Adjustment |
| 27.53 | 0.05% |
| 35.00 | 0.07% |
| 39.11 | 0.09% |
| 63.25 | 0.18% |
| 83.20 | 0.89% |
| 100 | 1.68% |
Requesting a Targeted Review
If you believe an error was made in the calculation of your 2020 MIPS payment adjustment, you can request a targeted review from CMS via a QPP account through September 30, 2019, at 8:00 pm EST. A targeted review should be requested at the same level as you reported MIPS (individual or group).
CMS is encouraging MIPS clinicians and groups to submit a request as soon as possible if they can provide supporting documentation that a targeted review is warranted. A few examples of reasons for requesting a targeted review:
- Measure or Activity Issues - A MIPS eligible clinician or group has supporting documentation that there are calculation errors regarding measures or activities submitted during the reporting period.
- Extreme and Uncontrollable Circumstances - A MIPS eligible clinician or group has supporting documentation indicating that they should qualify for automatic reweighting of performance categories due to extreme and uncontrollable circumstances.
- Eligibility and Special Status Issues - A MIPS eligible clinician or group has supporting documentation indicating that certain errors were made, such as eligibility being wrongly assigned to the MIPS eligible clinician or group (e.g. the MIPS eligible clinician or group fell below the low-volume threshold and should not have received a payment adjustment) or they were excluded from the APM participation list and should have been scored under the APM scoring standard.
More information on how to request a Targeted Review can be found here.
Preparing for your 2019 MIPS Reporting
Clinicians should review their 2018 MIPS performance feedback which includes final MIPS scores and payment adjustment information. Any payment adjustments will apply towards your 2020 Medicare Part B payments for professional covered services. MDinteractive can obtain the reports for you and send you feedback on the data. Understanding your 2018 performance can offer valuable information on how you can make improvements for the new reporting year. If you have any questions regarding your 2018 feedback reports or need help with your 2019 MIPS reporting, please contact one of our MIPS specialists today.
Leave a comment