
What’s Included in Your Final MIPS Performance Feedback
Your 2024 MIPS Performance Feedback includes all data submitted or calculated for an individual clinician, group, or APM Entity under Traditional MIPS, a MIPS Value Pathway (MVP), or the APM Performance Pathway (APP).
Your feedback report includes:
- Final MIPS score
- Category-level scores and weights
- Bonus points (e.g., complex patient, small practice)
- Measure-level and activity-level performance data
- Improvement scoring
- Payment adjustment information
- Supplemental administrative claims reports
- Comparative quality and cost feedback (for MVPs)
How to Access Your 2024 MIPS Final Scores and Payment Adjustments
Authorized users (clinicians, group representatives, and APM Entity contacts) can view feedback through the QPP website:
- Log in at https://qpp.cms.gov.
- Click "View PY 2024 Final Performance Feedback" or select "Performance Feedback" from the left-hand navigation pane.
- Choose your organization (Practice, APM Entity, or Virtual Group).
Accessing Your Feedback in MDinteractive
If you use MDinteractive for your MIPS reporting:
- Already granted access? Your 2024 reports are uploaded to your account. Click the green “QPP Performance Feedback” icon on your MIPS dashboard, then select “2024 QPP Feedback.”
- Need to grant access?
- Create a QPP HARP account (if you don’t already have one).
- Log in to your MDinteractive account at www.mdinteractive.com
- Click the blue “QPP Performance Feedback” icon on your dashboard and follow the prompts.
APM Entities
APM Entity representatives with Staff User or Security Official roles can view final scores for their Entity. Medicare Shared Savings Program ACO representatives can access their MIPS feedback using the ACO Management System (ACO-MS) credentials.
Understanding Your Final MIPS Score
Your final MIPS score combines the four performance categories and any applicable bonuses, such as the complex patient bonus. If you participated in MIPS in multiple ways (e.g., both group and individual levels), CMS assigns the highest possible score for your TIN/NPI combination.
2024 Category Weights:
- Quality – 30%
- Cost – 30%
- Improvement Activities – 15%
- Promoting Interoperability – 25%
If CMS couldn’t score you on a category—or if special circumstances applied, such as a special status designation for Promoting Interoperability reweighting, a hardship exception, or an Extreme and Uncontrollable Circumstances (EUC) exception—that category’s weight was redistributed to the remaining performance categories.
Detailed Components Explained
Cost Category
If your feedback shows “N/A” for Cost, you were not scored on any Cost measures due to case minimums not being met or reweighting. If you met the minimum case threshold, you can still review measure-level and patient-level feedback for Cost measures.
Note: The Acute Kidney Injury Requiring New Inpatient Dialysis measure will not be scored for the CY 2024 performance period / 2026 payment year.
Patient-Level Reports
These reports list the specific patients included in the calculation of your administrative claims-based Quality and Cost measures.
Complex Patient Bonus
Clinicians, groups, or APM Entities with an average Hierarchical Condition Categories (HCC) risk score or dual eligibility ratio above the median earn a complex patient bonus.
Improvement Scoring
You can earn:
- Up to 10 bonus points in the Quality category for year-over-year improvement.
- Up to 1 bonus point in Cost for improvement from the previous year.
Facility-Based Scoring
If your Quality and Cost scores are derived from facility-based scoring, you won’t see measure details. Instead, CMS will display your Hospital VBP Program score and MIPS-equivalent score.
2026 Payment Adjustments
Your final 2024 MIPS score determines your 2026 Medicare Part B payment adjustment, applied on a sliding scale relative to the performance threshold. MIPS payment adjustments are budget neutral—the total positive adjustments cannot exceed the total negative adjustments.
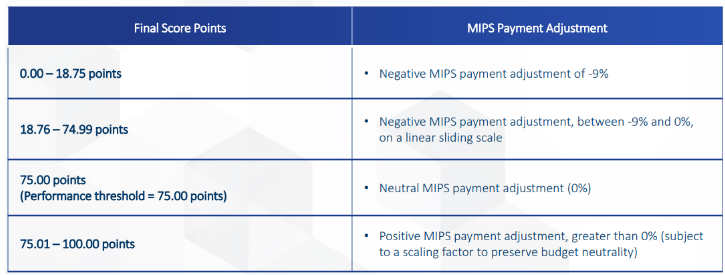
2026 Payment Adjustment Range:
- Negative adjustment: up to –9%
- Positive adjustment: up to +1.05% (for a perfect score of 100)
Examples of estimated payment adjustments based on 2024 MIPS final scores:
| 2024 Final Score | Estimated 2026 Payment Adjustment |
|---|---|
| 100 | 1.05% |
| 90 | 0.63% |
| 80 | 0.21% |
| 75 | 0% |
| 60 | -1.73% |
| 50 | -2.89% |
| 40 | -4.04% |
| 30 | -5.20% |
| 20 | -6.36% |
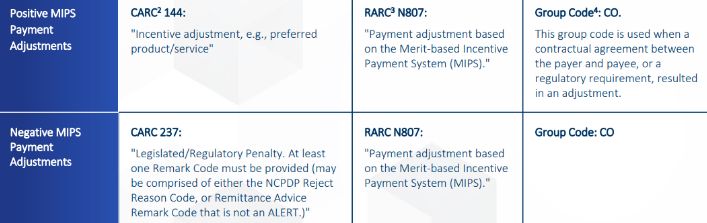
If a payment adjustment applies, the Remittance Advice (RA) will include relevant MIPS payment codes.
How to File a Targeted Review
You can request a Targeted Review through your QPP account until November 14, 2025, at 8 p.m. ET. File at the same reporting level (individual or group) used for submission. CMS recommends submitting as soon as possible if errors are identified.
CMS recommends filing if:
- Your data was submitted under the wrong TIN or NPI.
- You qualified for a hardship exception or reweighting that wasn’t correctly applied.
- You believe there’s an error in your payment adjustment calculation.
Once the deadline passes, you cannot appeal your score—so review your feedback as soon as possible.Once the deadline passes, you cannot appeal your score. Contact the QPP Service Center at 1-866-288-8292 or email QPP@cms.hhs.gov.
Next Steps
Check your 2024 MIPS feedback today and file a Targeted Review if you believe there’s an error in your score or payment adjustment. MDinteractive can help you:
- Access your CMS feedback reports
- Interpret your MIPS results
- Plan your 2025 MIPS reporting strategy
MIPS reporting requirements continue to evolve—so early preparation is key. Log in to your MDinteractive account to begin your 2025 MIPS reporting plan today.
Leave a comment