
Accountable Care Organizations (ACOs) participating in the Medicare Shared Savings Program (MSSP) will be required to report electronic clinical quality measures (eCQMs) or MIPS CQMs beginning in 2025 after the CMS Web Interface sunsets. The shift towards a new reporting method has significant implications for ACOs, so understanding how quality will be reported and assessed is critical. In this article, we will cover what ACOs need to know about the new reporting requirements and why gaining early experience with the measures can lead to better reporting results in the future.
Timeline for ACO Quality Measurement Changes
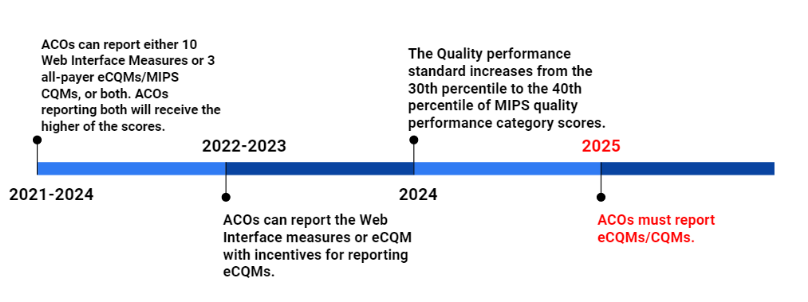
The Centers for Medicare and Medicaid Services (CMS) is revamping how MSSP ACOs report and are measured on quality. CMS will retire the Web Interface as a reporting option for ACOs in 2025. Beginning that year ACOs will be required to report eCQMs or MIPS CQMs. This new reporting framework called the APM Performance Pathway (APP), is intended to improve the quality of patient care and better align ACO quality reporting with the Quality Payment Program (QPP) Merit-Based Incentive Payment System (MIPS).
CMS delayed the mandatory transition to eCQMs or MIPS CQMs in response to ACO concerns, making it optional for reporting years 2021 through 2024. During the transition period, ACOs can choose to report:
- The CMS Web Interface measure set; or
- Three eCQMs/MIPS CQMs; or
- Dually report both the Web Interface measure set and the eCQMs/MIPS CQMs and receive the higher of the two scores.
The APP Measure Set and Scoring Methodology
The APP measure set includes three clinical quality measures, two administrative claims measures (the Hospital-Wide, 30-day, All-Cause Unplanned Readmission Rate and Clinician and Clinician Group Risk-standardized Hospital Admission Rates for Patients with Multiple Chronic Conditions), and the Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS Survey. The quality measures will assess the quality of patient care for diabetes, depression, and hypertension.
| Measure | Description | Specifications | |
|---|---|---|---|
| #1 (CMS122) Diabetes Mellitus: Hemoglobin A1c Poor Control | Reported for patients aged 18-75 with diabetes who had hemoglobin A1c > 9.0% during the measurement period. | CQM | eCQM |
| #134 (CMS52) Screening for Depression and Follow-up Plan | Reported for patients aged 12 years and older screened for depression on the date of the encounter or 14 days prior to the date of the encounter using an age-appropriate standardized depression screening tool AND if positive, a follow-up plan is documented on the date of the eligible encounter. | CQM | eCQM |
| #236 (CMS165) Hypertension (HTN): Controlling High Blood Pressure | Reported for patients aged 18 - 85 who had a diagnosis of hypertension overlapping the measurement period and whose most recent blood pressure was adequately controlled (< 140/90 mmHg) during the measurement period. | CQM | eCQM |
eCQMs vs MIPS CQMs
ACOs must select to report the three quality measures as either eCQMs, which include data generated from certified electronic health record (EHR) technology, or MIPS CQMs, which are calculated and reported by a Qualified Registry. The difference between eCQMs and MIPS CQMs comes down to the source of the data.
| eCQM Data Sources | CQM Data Sources |
|---|---|
|
|
*Quality Reporting Document Architecture
MDinteractive is a CMS Qualified Registry and is certified by the Office of the National Coordinator for Health Information Technology (ONC) to generate eCQMs. We can process and report both eCQMs and MIPS CQMs through the APP.
The reporting methodology for ACOs will move from a sample-based reporting approach to reporting “all-payer” data. ACOs have historically reported each quality measure under the Web Interface for a sample of 248 Medicare-assigned beneficiaries. In contrast, reporting eCQMs or MIPS CQMs will involve reporting a broader patient population. ACOs will have to meet new “data completeness” requirements meaning each measure must be reported on at least 70% of eligible patients, regardless of payer, from all clinicians participating in the ACO (including specialists). This threshold increases to 75% in 2024.
Further guidance from QPP can be found on this document.
APP Measure Scoring
ACOs will receive a score of between 3 to 10 points for each measure that meets the data completeness and case minimum requirements. The number of points an ACO earns for each measure will be based on the ACO’s performance compared to benchmarks that are used for other non-ACO individual and group reporters under the MIPS program. Benchmarks will be specific to the selected reporting method (eCQMs vs MIPS CQMs).
Beginning in 2023, a health equity adjustment will reward ACOs that report all-payer eCQMs/MIPS CQMs, are high performing, and serve a high proportion of underserved beneficiaries. The adjustment would add up to 10 bonus points to the ACO’s MIPS quality performance category score.
Quality Performance Standard
CMS has also altered the quality performance standard threshold, which is the minimum quality score an ACO must meet in order to be eligible to earn any shared savings. The performance standard is the 30th percentile of MIPS quality scores for 2021 through 2023, and the 40th percentile for 2024 and later years.
Beginning in 2023, ACOs scoring below the minimum quality performance standard will be eligible for shared savings (or owe shared losses) at a lower rate if they score at the 10th percentile or above on at least one of the four APP outcome measures. The lower rates of shared savings/losses will be calculated on a sliding scale tied to the ACO’s quality performance score.
| ACO Quality Performance Standard | |||
|---|---|---|---|
| 2022 | 2023 | 2024 | 2025 |
|
|
|
|
*Excludes entities/providers eligible for facility-based scoring.
If an ACO does not report either the CMS Web Interface measure set or the three eCQMs/MIPS CQMs in 2023 or 2024, or the three eCQMs/MIPS CQMs in 2025, and administer a CAHPS survey each year, they will not meet the quality performance standard or the alternative performance standard.
CMS calculates the 30th or 40th percentile scores based on the distribution of all MIPS quality performance category scores for the applicable performance year, so estimates for the percentile scores for 2022 (and beyond) will not be available until after the end of the reporting period. The historical unweighted MIPS Quality performance category scores for the 2018-2021 performance years should serve as a guide for estimating quality performance scores. For 2021, the MIPS Quality performance category score at the 30th percentile was equivalent to 61.73 out of 100. This means that ACOs should focus on achieving at least 6.173 MIPS points on each of the 6 APP measures.
| Historical Unweighted MIPS Quality Performance Category Scores | ||
|---|---|---|
| Performance Year | 30th percentile of the MIPS Quality performance category score | 40th percentile of the MIPS Quality performance category score |
| 2018 | 59.30 | 70.80 |
| 2019 | 58.00 | 70.82 |
| 2020 | 63.90 | 75.59 |
| 2021 | 61.73 | 77.83 |
Why Starting Early is Important
Preparing for the new data reporting requirements will take time due to the complexity involved in the transition to eCQM and MIPS CQM reporting. ACOs will have to develop workflows and the necessary infrastructure to aggregate data across all of their Tax Identification Numbers (TINs), electronic health record systems (EHRs), billing systems, and other clinical data platforms in order to be able to capture and report all-payer data. They will also have to ensure the data is de-duplicated for reporting purposes.
The voluntary transition period gives ACOs time to address all-payer data aggregation challenges and the opportunity to gain experience with eCQMs and MIPS CQMs before the new reporting requirements become mandatory in 2025. It also allows ACOs to learn how they are performing so they can start trying to improve their scores. ACOs getting to work on eCQM and MIPS CQM reporting early should start by considering the 5 Ws below:
- Who are your eligible patients? An ACO should first tackle identifying its eligible patient population for each of the quality measures (e.g., how many diabetic patients are from each of its TINs and practices?). Completing a preliminary analysis of the eligible population will allow ACOs to concentrate on TINs that have the majority of eligible patients.
- Where is your data? ACOs need to assess where all of the relevant data is located across their ACO which can include multiple TINs, EHRs, billing systems, and other data platforms. A recent survey of the NAACOS membership found that only 17 percent of respondents use one EHR, 24 percent use two-to-five different EHRs, and 20 percent use between six and 10 different EHRs. Reconciling data across disparate resources can be a challenge, so it is important to have effective aggregation tools in place to support this process.
- What is your performance? The number of patients that met/did not meet performance for the measure(s) will have to be calculated on at least 70% of the eligible patients. After the data completeness threshold has been met, the ACO can calculate and review the approximate performance rate for each measure.
- When do you report the data? Data must be collected for all 12 months of the performance year (January 1st through December 31st). The submission deadline is March 31st following the end of the performance period if the ACO decides to submit data to CMS during the transition period.
- Why should you use the transition period to start early? ACOs will need to perform well on the measures to ensure eligibility for shared savings. Understanding what performance looks like on the eCQMs or MIPS CQMs now will give ACOs time to make any workflow and operational changes that are needed to improve their performance. Also, CMS will allow lower scores on the APP measures for ACOs voluntarily reporting during the transition period.
Next Steps
ACOs have only a couple of more years to prepare for eCQM and MIPS CQM reporting before it becomes mandatory in 2025. MDinteractive offers cost-effective solutions for aggregating data from multiple sources, data validation, and tracking performance. Gaining this experience now is the best way to ensure future reporting success. Schedule a meeting to learn more how MDinteractive can help your ACO successfully navigate eCQM and CQM reporting.
Leave a comment