
The MIPS Cost category weight is increasing to 20% of a clinician’s final MIPS score in 2021 and 30% in 2022. The increase reflects the priority that the Center for Medicare and Medicaid Services (CMS) has placed on controlling the cost of health care services as a component of the MIPS program. As Cost makes up a larger portion of the total MIPS score, it’s beneficial to understand how CMS measures Cost. Let’s review the basic components of the Cost category and examine strategies to manage and potentially improve performance.
MIPS Cost Category Overview
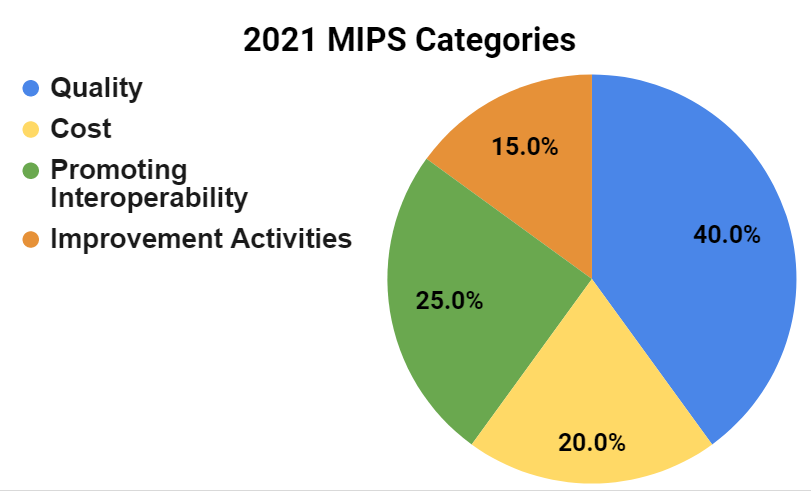
CMS uses the Cost category to measure Medicare payments made for care provided to patients. The Cost category is one of four performance categories under the MIPS program that can contribute to the final MIPS score. It’s that final MIPS score that determines a clinician’s Medicare payment adjustment. The weight of the Cost category has been steadily increasing since the inception of the MIPS program and will represent 20% of a clinician’s total MIPS score in 2021. By law, the Quality and Cost performance categories must be equally weighted at 30% beginning with the 2022 performance period.
Note: The Cost Category is weighted at 0% for Alternative Payment Model (APM) Entities.
The Cost category has a 12-month performance period (January - December). It compares the cost of care provided to patients who are attributed to a MIPS eligible clinician or group to a national benchmark. Unlike the other MIPS categories that require performance data to be reported to CMS (e.g., Quality, Promoting Interoperability and Improvement Activities), the Cost score is automatically calculated by CMS using Medicare Part A and B claims data submitted during the MIPS performance year. This means that there are no data submission or reporting requirements for clinicians and groups for the Cost category beyond their routine Medicare claim submissions.
MIPS Cost Measures
There are a total of 20 Cost measures available for the 2021 MIPS performance year. CMS uses Cost measures to assess the overall cost of care provided to Medicare patients during the year with a focus on:
- The primary care they received;
- The cost of services provided to Medicare patients related to a hospital stay; and
- Costs for items and services provided during 18 episodes of care for Medicare patients.
The measure type determines how the cost is attributed to a clinician based on the measure’s unique specifications. Each Cost measure has specific eligible case minimums that must be met for a clinician to be scored on the measure.
| Measure Name | Description | Case Minimum |
|---|---|---|
| Total Per Capita Cost (TPCC) | Assesses the overall cost of care delivered to a Medicare patient with a focus on primary care received. | 20 Medicare patients |
| Medicare Spending Per Beneficiary Clinician (MSPB Clinician) | Assesses the cost of care for services related to qualifying inpatient hospital stay (immediately prior to, during, and after) for a Medicare patient. | 35 episodes |
| 18 Episode-based Cost Measures (13 procedural measures and 5 acute inpatient medical condition measures) | Assesses the cost of care that is clinically related to the initial treatment of a patient and provided during an episode’s timeframe. | -20 episodes for acute inpatient condition episode-based measures -10 episodes for procedural episode-based measures |
CMS did not add any new episode-based Cost measures in 2021 but did include telehealth services in the current cost measure calculations, as applicable. The episode-based measures are categorized into “episode groups” (e.g., procedural episodes or acute inpatient medical condition episodes). All of the episode-based Cost measures are listed below:
Procedural episode-based measures
- Elective Outpatient Percutaneous Coronary Intervention (PCI)
- Knee Arthroplasty
- Revascularization for Lower Extremity Chronic Critical Limb Ischemia
- Routine Cataract Removal with Intraocular Lens (IOL) Implantation
- Screening/Surveillance Colonoscopy
- Acute Kidney Injury Requiring New Inpatient Dialysis
- Elective Primary Hip Arthroplasty
- Femoral or Inguinal Hernia Repair
- Hemodialysis Access Creation
- Lumbar Spine Fusion for Degenerative Disease, 1-3 Levels
- Lumpectomy Partial Mastectomy, Simple Mastectomy
- Non-Emergent Coronary Artery Bypass Graft (CABG)
- Renal or Ureteral Stone Surgical Treatment
Acute inpatient medical condition episode-based measures
- Intracranial Hemorrhage or Cerebral Infarction
- Simple Pneumonia with Hospitalization
- ST-Elevation Myocardial Infarction (STEMI) with Percutaneous Coronary Intervention (PCI)
- Inpatient Chronic Obstructive Pulmonary Disease (COPD) Exacerbation
- Lower Gastrointestinal Hemorrhage (applies to groups only)
MIPS Cost Scoring
MIPS eligible clinicians and groups will be evaluated and scored on each Cost measure for which they meet or exceed the established case minimum requirements during the performance year. If any of the measures do not have enough attributed Medicare beneficiaries, then the remaining measures are averaged to calculate the score.
Each measure is scored out of 10 possible points. CMS assigns points for the Cost measures by comparing the clinician or group’s performance on a measure to a benchmark that is established during the performance year rather than historic benchmarks.
If clinicians don’t meet the case minimum requirements and don’t receive a score for any Cost measures, the Cost category will be reweighted to the Quality category (making Cost 0% of the final MIPS score and Quality 60% of the final MIPS score).
What Clinicians Can Do to Improve Their Cost Performance
While the Cost category is not a reportable category, there are some things clinicians can do to manage their costs and performance:
- Review your past performance. If you meet the case minimum requirements for any of the cost measures you will receive category and measure-level scoring information in your CMS Performance Feedback Reports. CMS typically releases the reports during the summer after the performance year. It is recommended that you review your past reports as they can assist with estimating your possible scores for 2021 and beyond. MDinteractive can help with accessing your CMS Performance Feedback Reports and interpreting the results. Log into your MDinteractive account and click the “QPP Performance Feedback” button to give us permission to access your reports from CMS.
- Focus on patient care coordination. Clinicians who better coordinate care can improve health outcomes while ensuring quality health care is provided in appropriate settings. Strategies to consider:
- Implement agreements with other clinicians for receiving patient information after they provide care to your patients.
- Educate patients on communicating with their other clinicians about the need to send their information to you.
- Use electronic referral capabilities.
- Encourage patients to bring in their medications for appropriate medication management.
- Bill using diagnosis codes that match patient complexity. CMS considers comorbid conditions when calculating the cost of care for beneficiaries whose care and treatment are more complex, but you need to ensure that your medical records and claims are coded correctly to accurately reflect patients' medical complexity. Hierarchical condition category (HCC) coding is a risk-adjustment model originally designed to estimate future health care costs for patients. The hierarchical condition category relies on ICD-10 coding to assign risk scores to patients. Each HCC is mapped to an ICD-10 code. A patient with multiple chronic conditions is expected to have higher health care utilization and costs. For example, a Type 2 Diabetes with no Complications (ICD10 E11.9) has a lower risk score than a Type 2 Diabetes with diabetic polyneuropathy (ICD10 E11.42). Note that CMS calculates the risk scores each year based on the diagnosis submitted during the reporting year. If a patient has diabetic polyneuropathy but CMS didn’t get the correct ICD10 in 2021, the risk score will not be adjusted by CMS.
- Take note of social determinants of health (SDOH). Identifying SDOH is critical to reducing healthcare costs and unnecessary utilization:
- Use Z codes to capture data on the social needs of your patient population. Z codes identify non-medical factors that may influence a patient’s health status.
- Identify support services for referral for vulnerable patients.
- Acknowledge and address health disparities.
- Consider using a standardized patient risk assessment tool to better understand patients’ SDOH such as The Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) toolkit.
- Pay attention to emergency room visits and hospital readmissions. Preventable emergency room visits and hospital readmissions contribute to higher utilization and costs. Clinicians can educate patients on appropriate levels of care by providing access to same-day office visits, telehealth visits, or an after-hours phone line. Hospital admissions/discharge/transfer (ADT) notifications are another way clinicians can stay updated on a patient’s status so they can steer those patients toward appropriate interventions. The ADT system also helps identify inappropriate use. These combined efforts will reduce overutilization by preventing avoidable emergency room visits and hospital readmissions.
- Focus on preventive care and disease management. Primary care clinicians can use the annual wellness visits to capture and record chronic conditions and develop a plan to support patients to better manage their disease. Likewise, specialists can encourage patients with chronic conditions to see their primary care clinicians.
Summary
The Cost category is evolving and becoming a more important part of your total MIPS score. Paying closer attention to how Cost measures are scored can help you identify opportunities to make improvements within your practice if necessary. There are a variety of strategies you can consider within your practice to impact your Cost performance. The first step is reviewing your CMS Feedback Reports to better understand your past performance. The MDinteractive team is available to assist you with accessing your prior QPP Performance Feedback Reports and providing insight on the results.
Leave a comment