All Improvement Activities (IA) can be easily attested to with MDinteractive.
- Log into your account
- Click on Add/Edit next to the IA category. This will direct you to the IA reporting module. Note that you might have to enter your NPI/TIN combination or just TIN (if reporting as a group) to be able to see the categories and Add/Edit.
- Enter your minimum 90 day reporting period
- Click “Add” to each activity that you performed for at least 90 consecutive days:
Note: There are frequency restrictions associated with the following Improvement Activities: IA_PSPA_4, IA_PSPA_22, IA_PSPA_23, and IA_PSPA_24. Please review documentation/rules for these activities prior to attesting to them in 2020.
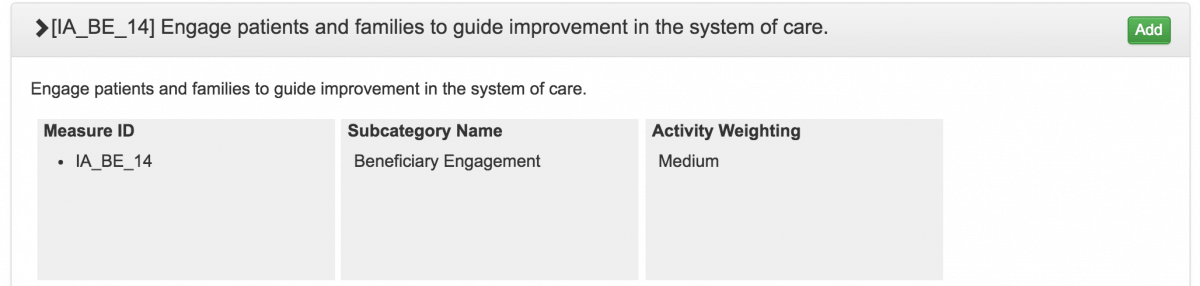
Each activity is weighted either medium or high.
To achieve the maximum 40 points for the Improvement Activity score:
A clinician (that works in a group with 15 or fewer providers billing with the same TIN) may select either of these combinations:
- 1 high-weighted activity OR
- 2 medium-weighted activities
Clincians working on larger groups will need to attest to more activities to receive full credit for this category:
- 2 high-weighted activities OR
- 1 high-weighted activity and 2 medium-weighted activities OR
- 4 medium-weighted activities