
Part 2 of our Mastering MIPS series, reviews the Quality performance category in the traditional Merit-Based Incentive Payment System (MIPS). The 2023 MIPS reporting year is now half over, so clinicians should already be proactively collecting and reporting data on their Quality measures. In this blog, we will cover important topics about the Quality category, including an overview of the Quality reporting requirements in 2023, how Quality measures are scored, and tips for clinicians to select the best Quality measures for their practice.
The MIPS Quality Category
The MIPS Quality category evaluates how well clinicians and groups perform on quality measures used to assess various aspects of healthcare, including healthcare processes, outcomes, and patient experiences of care. It is one of four performance categories under the MIPS program. Each category awards a certain number of points depending on its weight.
Quality is weighted differently based on the size of the practice:
- 30% of the total MIPS score for large practices (16 or more NPIs).
- 40% of the total MIPS score for small practices (15 or fewer NPIs) that do not report the Promoting Interoperability (PI) category.
*MIPS category weights may change based on special statuses, exception applications, or reweighting of other performance categories.
What are the MIPS Quality Category Reporting Requirements?
The 2023 Quality reporting requirements are generally the same as last year. The one major exception is a new reporting option called the MIPS Value Pathway (MVP). More information about MVPs can be found here.
- Select six measures (including an outcome or a high-priority measure) or a specialty measure set or a MIPS Value Pathway (MVP). NOTE: MVPs are a new reporting option in 2023. If reporting an MVP four quality measures are selected from the list of measures in the MVP (one must be an outcome or a high-priority measure).
- Collect and report data for all 12 months of the performance year (January-December).
- Report at least 70% of eligible encounters for all insurances (includes Medicare and non-Medicare).
In certain cases, clinicians can report less than six measures through the Eligible Measures Applicability (EMA) Process. Under EMA, for example, an anesthesiologist may only need to report four quality measures (404, 424, 430, and 463) with a registry. Some specialty measure sets may also have fewer than 6 measures to report. If reporting the Hospitalist Specialty measure set, for example, only 4 Quality measures must be reported (#5, #8, #47, and #130).
What Quality Measures are Available to Report in 2023?
A total of 198 quality measures are available for reporting this year. CMS publishes changes to the Quality measure inventory at the start of each new performance year. For example, nine new measures are available to report in 2023 and 11 measures were retired. An additional two measures were partially removed (#110 and #111) and can only be reported within the new MVPs. New measures and retired measures are listed in the tables below.
| 2023 Retired Measures |
|---|
| #76 Prevention of Central Venous Catheter (CVC) - Related Bloodstream Infections |
| #110: Preventive Care and Screening: Influenza Immunization (only available for MVP reporting) |
| #111: Pneumococcal Vaccination Status for Older Adults (only available for MVP reporting) |
| #119 Diabetes: Medical Attention for Nephropathy |
| #258 Rate of Open Repair of Small or Moderate Non-Ruptured Infrarenal Abdominal Aortic Aneurysms (AAA) without Major Complications (Discharged to Home by Post-Operative Day #7) |
| #265 Biopsy Follow-Up |
| #323 Cardiac Stress Imaging Not Meeting Appropriate Use Criteria: Routine Testing After Percutaneous Coronary Intervention (PCI) |
| #375 Functional Status Assessment for Total Knee Replacement |
| #425 Photodocumentation of Cecal Intubation |
| #455 Percentage of Patients Who Died from Cancer Admitted to the Intensive Care Unit (ICU) in the Last 30 Days of Life (lower score – better) |
| #460 Back Pain After Lumbar Fusion |
| #469 Functional Status After Lumbar Fusion |
| #473 Leg Pain After Lumbar Fusion |
Clinicians should choose quality measures that best fit their practice, including the type of care they provide and the clinical conditions they typically treat. The full list of Quality measures can be found on MDinteractive’s website here or a list by specialty here. Customized suggestions are also available directly when logged into an MDinteractive account based on a clinician’s prior Medicare billing data.
Have Any Quality Measures Changed?
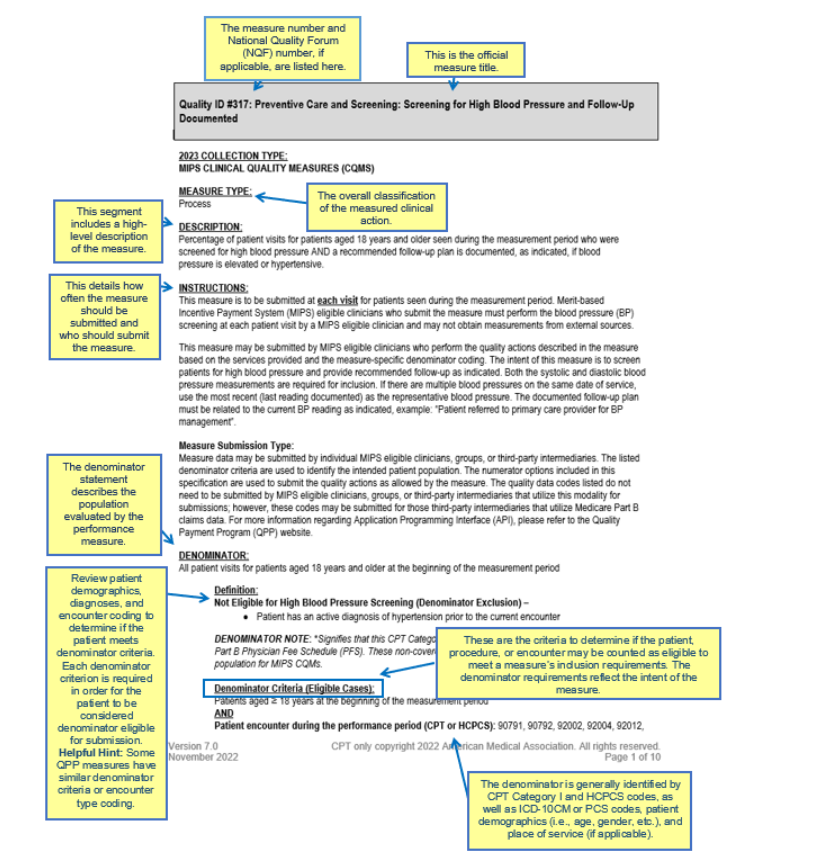
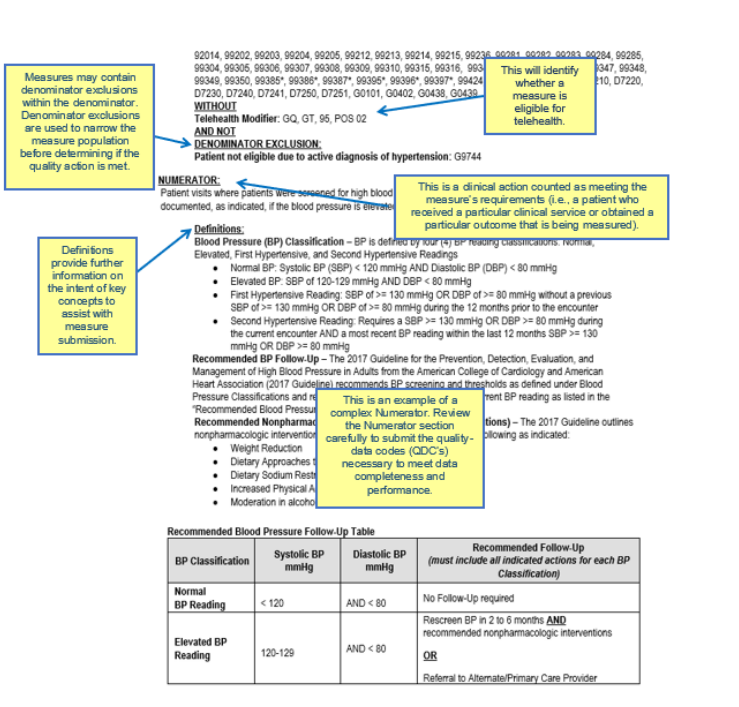
Every quality measure comes with its own set of specifications, which may also undergo changes from year to year. The individual measure specifications are detailed descriptions of the quality measures and include important instructions for reporting each measure, including:
- How frequently the measure should be reported (e.g., once per year or at “every” visit).
- The unique eligible population to report (denominator) based on billing codes, diagnosis codes, and other patient demographics (e.g., age, gender, etc.).
- How to comply with the measure (the defined quality actions) for the eligible population (numerator).
The CMS diagram below explains how to read the CMS documentation for a Quality measure.
CMS made substantive changes to 76 quality measures for the 2023 performance year. Clinicians should carefully review the measure specifications to ensure they are reporting each measure correctly. Below are a few examples of changes for some commonly reported measures.
- Measures #5 Heart Failure (HF): Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor Blocker (ARB) or Angiotensin Receptor-Neprilysin Inhibitor (ARNI) Therapy for Left Ventricular Systolic Dysfunction (LVSD), #7: Coronary Artery Disease (CAD): Beta-Blocker Therapy – Prior Myocardial Infarction (MI) or Left Ventricular Systolic Dysfunction (LVEF ≤ 40%), and #008: Heart Failure (HF): Beta-Blocker Therapy for Left Ventricular Systolic Dysfunction (LVSD)
- CMS updated the denominator (eligible population) for these measures from left ventricular ejection fraction (LVEF) less than 40% to LVEF less than or equal to 40%.
- Measure #181: Elder Maltreatment Screen and Follow-Up Plan
- The denominator (eligible population) now includes all patients aged 60 years and older.
- #374: Closing the Referral Loop: Receipt of Specialist Report
- Beginning in 2023 only the first referrals made between January 1 - October 31 (the measurement period) will count towards the denominator.
- #439: Age-Appropriate Screening Colonoscopy
- The age requirements for the denominator changed to include all screening colonoscopy examinations performed on patients aged 45 years and older.
- Measures #459: Back Pain After Lumbar Surgery, #461: Leg Pain After Lumbar Surgery, and #471: Functional Status After Lumbar Surgery
- CMS added Submission Criteria 2 (Patients with lumbar fusion procedure) to each of the measures.
How Are Quality Measures Scored?
CMS will score the top 6 Quality measures, including at least 1 Outcome or High Priority measure. The number of points awarded for a Quality measure will depend on various factors.
| 2023 Quality Measure Scoring Policies | |
|---|---|
| 1-10 points | Measures can generally earn between one and ten points based on a clinician or group’s performance if the measures have a benchmark, meet data completeness (70% of eligible cases reported), and meet case minimum requirements (at least 20 eligible cases for the year).* Note: Some “topped out” measures are capped at 7 points. |
| 7 points |
New measures in their first year have a scoring floor of seven points.
This scoring floor applies to new measures #485 – #493 that were added to the program in the 2023 performance period. |
| 5 points |
New measures in their second year have a scoring floor of five points.
This scoring floor applies to measures #481 – #483 that were added to the program in the 2022 performance period. |
| 0 points | Measures will earn zero points if data completeness and case minimum requirements aren’t met, or if the measure has no benchmark (small practices will continue to earn three points).* |
*These scoring policies don’t apply to new measures during the first 2 performance periods available for reporting.
How Do Benchmarks Impact Measure Scoring?
Quality measures are assessed against their benchmark to determine how many points the measure receives based on the clinician or group’s performance. Each measure has its own benchmark that is specific to the collection type: Qualified Clinical Data Registry (QCDR) measures, MIPS Clinical Quality Measures (MIPS CQMs)*, electronic CQMs (eCQMs), CMS Web Interface measures, the Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey, and Part B Claims measures. For quality measures with no historical benchmark, CMS may calculate a benchmark based on 2023 data post-submission if CMS collects sufficient data during the performance period.
A “topped out” measure is one where the national median performance rate is so high that there is no meaningful difference in performance between clinicians. Some topped-out measures are capped at seven points (versus 10 points) and can make it harder to optimize Quality category scores.
Clinicians should closely examine the measure benchmarks to understand the scoring implications for the measures they plan to report. All 2023 measure benchmarks can be found here.
Tips for Selecting Measures
Here are some tips for clinicians to consider when selecting Quality measures to report in 2023:
- Review Measure Relevance: Assess the relevance of each measure to your practice and unique patient population. Focus on measures that align closely with your specialty and the services you provide.
- Prioritize High-Impact Measures: Identify measures that have a significant impact on patient outcomes and healthcare quality and that have high-scoring potential. You may want to consider reporting new measures introduced in 2023 that have a higher scoring floor.
- Consider Data Volume: Evaluate the feasibility of collecting and reporting data for each measure based on the CMS documentation, paying careful attention to the eligible population you must report and how frequently the measure must be reported. Choose measures that can be easily and reliably captured within your practice's workflow.
- Optimize Performance: Analyze your historical performance data to identify areas where you have excelled or areas that require improvement. Select measures that allow you to showcase your strengths or demonstrate progress in areas where you aim to enhance performance.
- Stay Informed: Keep up with updates and changes to MIPS measures and reporting requirements. Regularly review guidance from CMS to ensure you are aware of any modifications or new measures introduced.
- Plan for Long-Term Success: Look beyond the current reporting year and consider measures that align with your long-term quality improvement goals. Select measures that can help drive meaningful change and promote continuous enhancement of patient care.
Selecting the right Quality measures appropriate for your practice is the first step toward successful MIPS reporting. MDinteractive provides many resources to help you develop an effective MIPS reporting plan, including guidance on measure selection and suggestions to simplify your data collection and reporting efforts.
Leave a comment